- OT
- Professional support
- Health services
- Fortune telling
The cover story
Fortune telling
What does the future of optometry hold? From eye care close to home, to the skills optometrists need for extended roles, OT explores how the profession is transforming to deliver better patient care

10 December 2022
When Chaz Uppal considers the difference Optometry First is making within Bassetlaw, he thinks of the four-year-old he fitted with spectacles after being on a hospital waiting list for over a year with strabismus and a +8.00D prescription.

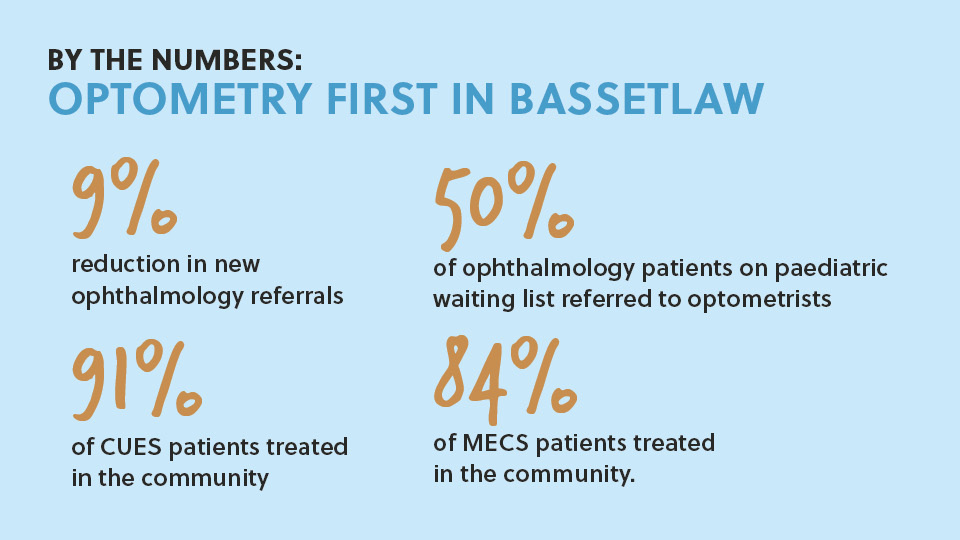
After Bassetlaw became an early adopter area for Optometry First – a national vision that brings eye care close to home – an audit was performed on the waiting list for paediatric care within ophthalmology.
Half of the children on the waiting list were redirected to optometry practices. A further audit of the adult waiting list for ophthalmology redirected one in five patients to the community.
“Now we have provision to offer community services, free up hospital appointment time and enable secondary care to concentrate on more complex cases. It should be done all over the country,” Uppal emphasised.
Uppal and clinical lead for the Local Optical Committee Support Unit, Nizz Sabir, began talks with the Bassetlaw clinical commissioning group in 2019. The pair put forward a plan for optometry to deliver a ‘basket of services’ instead of commissioning individual contracts.
“Due to the NHS sight test system not covering any further investigation of acute or chronic eye conditions we thought having a community services would better serve the patients at the point of contact and reduce waiting times within secondary care,” Uppal told OT.
This plan was agreed to and the services that were commissioned later fell under the banner of Optometry First.
In the wake of the pandemic, NHS trusts across the country faced growing waiting lists, with more than 600,000 patients waiting for ophthalmology treatment at the end of December 2021. Bassetlaw also faced significant challenges in delivering eye care.
“Operationally, it was a situation where we wanted to change,” Carolyn Fox, head of provider transformation for Optometry First, told OT.
“Whilst the pandemic was horrendous for everybody, what it really has done for the NHS is enable change,” she said.
“Within ophthalmology, the trust stood back and realised that they did not have the capacity to meet the demand. They wanted to do something differently,” Fox shared.
A shifting approach
Bassetlaw introduced the COVID-19 Urgent Eyecare Service (CUES) and a minor eye conditions service (MECS).
Of those patients who were seen in optometry practices through CUES, 91% were treated within the community. Within MECS, 84% were managed within primary care.
“It was then that optometrists said, ‘We can do more and we want to help you’,” Fox shared.

A referral refinement service sees referrals from optometrists to secondary care assessed by Primary Eyecare Services (PES) before reaching an ophthalmologist.
PES provides advice and guidance to the optometrist if there is insufficient information within the referral or it is thought to be better suited for primary care.
“They will signpost to the appropriate community service if there is one in Optometry First,” she said.
Since its introduction, there has been a 9% reduction in referrals to ophthalmology in the three months since it was introduced in July.
Operationally, it was a situation where we wanted to change
Consultant to consultant referrals within ophthalmology have also dropped by 32% over the same time period – meaning more referrals from primary care are being directed to the appropriate specialty.
“We have had word back from the trust that the quality of the referrals has changed as a result,” Fox said.
Looking ahead, there is potential for low-risk glaucoma patients and those requiring low vision services to be managed in the community.
“We have done the initial work around trying to close the front door and reduce demand. The next phase is really developing the relationship between ophthalmology consultants and optometrists to discharge out where appropriate,” Fox said.
Priceless care
Before Optometry First was introduced, Uppal would see patients in practice with conditions he had the skills and equipment to treat.
However, in the absence of a commissioned pathway patients would either have to pay privately or seek treatment at accident and emergency.
“Some optometrists were seeing patients free of charge – which is not financially sustainable,” Uppal said.
“From the patient’s perspective, it was their time of need, and we were trying to charge them. It was a very awkward conversation for us,” Uppal said.
Working in practice, Uppal has observed the anxiety created by lengthy waiting lists. He worries about the patients he has referred to secondary care who wait at home, with their vision continuing to deteriorate.
“Until they are diagnosed with a condition, they are in limbo,” Uppal said.
Uppal is now able to help ease the hospital backlog by seeing patients through a range of commissioned eye care services conveniently located on the High Street.
Through the Opera IT system, he is able to safely share images and video with secondary care, as well as access NHS summary care records.
Uppal mentions the case of a patient who presented in practice on a Friday afternoon and received surgery for a retinal detachment the following morning.
Until they are diagnosed with a condition, they are in limbo
“Secondary care saw the OCT scan and knew it had to be operated on. Without this service, that patient could have lost their vision,” Uppal said.
“That is the priceless bit,” he added.
Fox shared that in the context of the ongoing pressures created by COVID-19 and elective recovery efforts, hospitals need all the support that they can get.
“When you see the patients finally being treated – that is what motivates me,” she said.
The hurdles
The initial stages of rolling out Optometry First have not been without obstacles. As Local Optical Committee Support Unit clinical director, Zoe Richmond, shared with OT, while the early adopter areas were carefully selected “they weren’t cherry picked.”
“We have not avoided the challenging situations,” she said.
NHS England lead, Andy Byrne, highlighted that the main focus in Sefton has been conveying to secondary care what primary care optometry is capable of.
“We have moved the conversation forward and they now understand what optometrists can deliver,” he shared.
“We now need to get that contract up and running,” Byrne added.
The challenges in Sefton around engaging with secondary care are not unique to this area, he emphasised.
“Those challenges are understandable. Secondary care is equally passionate about their patients. They want to know they can send them to someone who will look after them. It is not a case of arrogance but lack of knowledge,” Byrne observed.
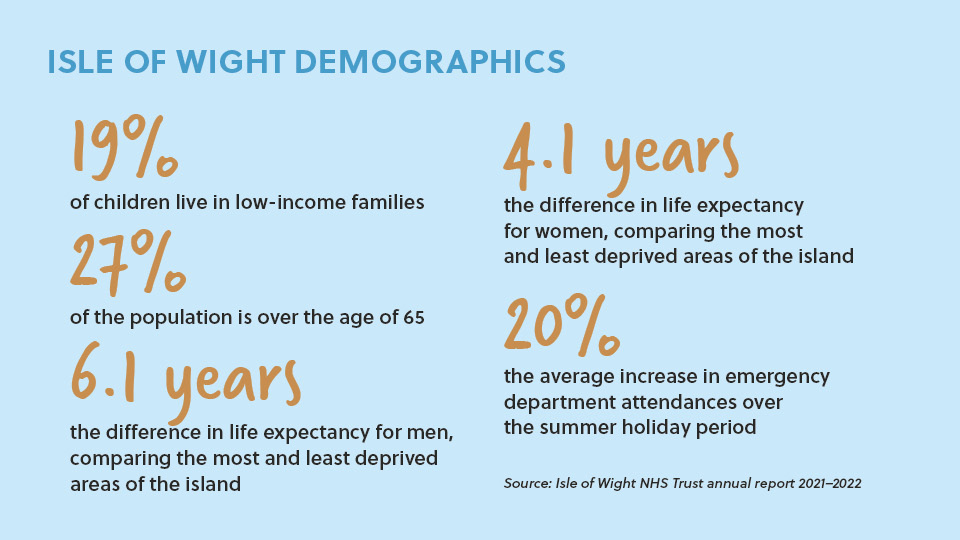
The demands of an ageing population are often highlighted in conversations about the future of eye care.

Tourists contribute to a flux in demand for healthcare services, with the trust reporting that there is typically a 20% increase in emergency department attendance during the summer holiday period.
“There is a lot of ebbing and flowing in the number of people who are on the island at any given time,” Hampshire Local Optical Committee chair, Bryony Allen, shared.
Allen believes that providing enhanced access to primary eye care through Optometry First will help to address health inequalities.
“Optometry First is about making everything a level playing field so that all optometrists in the future are able to deliver a standard of care and all patients will receive the same healthcare opportunities,” she said.
Within Allen’s role in professional services, she has observed regional disparities in what eye care services are commissioned within optometry.
Having that IT infrastructure that we can build on has been a real game changer for us
This creates training challenges for companies with staff in multiple locations, and also – in Allen’s view most importantly – results in confusion for patients.
“As an industry we are not able to give a single message to the public to say, ‘This is what optometry will do for you’,” she said.
“That confusion leads to patients returning to GPs and hospitals when perhaps they would be more appropriately supported with a community provider, “ Allen highlighted.
“In deprived areas it may lead to patients not accessing care at all due to patients not knowing where to go and worrying that it will cost them money,” she said.
Alongside the COVID-19 Urgent Eyecare Service, Optometry First has resulted in an integration of the software so that primary and secondary care can securely share patient information and images on the Isle of Wight.
“Having that IT infrastructure that we can build on has been a real game changer for us,” associate director of commissioning, Cheryl Harding-Trestrail told OT.
A pre-cataract pathway has been rolled out with a post-cataract pathway to be launched over the coming months.
Harding-Trestrail observed that in other areas the post-cataract appointment was rolled out first because it was more straightforward.
“What we have done with the island is think about the front of the pathway,” she said.
“If you say to someone already in hospital ‘You’re going to be followed up by an optometrist’ that is a slightly more broken pathway than starting at the beginning with the optometrist informing and educating the patient – giving them a real choice about their care,” she said.
In the future, there is potential for optometrists to play a role in glaucoma care, Harding-Trestrail added.
“In the fullness of time, we want people who are identified as having high intraocular pressure to be able to be managed in the primary care optometry service,” she said.
For senior commissioning manager, Donna Claydon, who had not worked within eye care before she started on Optometry First, the concept simply made sense.
“Why wouldn’t you tap into this skillset within optometry? We have ended up with something that is a changed foundation for the future – not just a pilot. It is something that we can carry forward,” she said.
Like Allen, Claydon believes that Optometry First will help to address disparities in access to eye care.
“Knowing that patients can go to an optometrist, who is qualified to an excellent standard, and receive free NHS access to care, breaks down some of the barriers which may have created inequality in the past,” she said.
A national vision
While Optometry First is gaining momentum at a local level, interviewees who spoke to OT emphasised the need for the model to gain traction nationally.
“It has been an honour to be an early adopter, but it doesn’t stop here. It is about a broader future – taking what we learn from this and building on it,” Allen told OT.
She added that progress through Optometry First on the Isle of Wight has inspired progress in other areas within Hampshire.
“We don’t want to reinvent the wheel. We want to take what already works and expand it in a wider area,” Allen said.
Fox noted that while significant progress has been made in Bassetlaw, it is relatively small – with 10 optometry practices and a population of 120,000 people.
Broader implementation would need to be supported by a “culture of change.”
“It is possible. A national mandate would be brilliant,” she shared.
Progress was made towards increasing the prominence of Optometry First on the national agenda in October at the second annual Westminster Eye Health Day.
During a tumultuous time in politics, a day before the resignation of Liz Truss, more than 40 MPs took time out of their diaries to hear a call for a national plan for eye care.
Minister of State for Health, Will Quince, acknowledged the work of Optometry First and said he would explore the potential to “turbo charge” the model.
“I want to see what services we can move from the hospital into the community. When I speak to most patients, what they say is, ‘I want my care to be close to home’,” he said.
Further learning
As extended clinical services are rolled out, the number of eye care professionals who continue to learn after qualification is increasing.
The 2021 General Optical Council registrant survey found that 40% of optometrists planned to gain an additional qualification over the next two years.
Optometrists involved in the delivery of extended eye care services were more likely to report plans for further learning over the period.
As an optometrist practising in an area with a glaucoma referral refinement scheme, Rukaiya Anwar welcomed the opportunity to complete a professional certificate in glaucoma.
The optometrist has undertaken qualifications in low vision, medical retina and independent prescribing.
“Optometry, despite what many people think, is a broad field with endless opportunities for specialisation. The eye is highly complex, and the more I practised, the more I wanted to learn,” Anwar said.
Completing higher qualifications gave Anwar increased confidence in providing well-rounded care to her community.

Reflecting on the beginning of her career, Anwar said that she initially thought she would never want to sit another exam after qualifying.
“How wrong was I? Passing your OSCEs is only the beginning. Find something that you are passionate about or interested in and explore further,” she emphasised.
When Suresh Munyal first qualified, he realised that he needed a different approach to learning than simply reading about pathology.
“I had a massive pile of magazines under my bed – the piles got bigger and I read them less and less,” Munyal shared.
“I decided that because of the way I was, the only way I was going to learn anything new was to be examined in it,” he said.
Alongside courses in contact lens fitting and independent prescribing, Munyal completed a business growth management course at Warwick University.
Learning has become more accessible since the days in the early 1990s when Munyal would drive to Bradford University after work to complete courses in paediatric care, contact lenses and abnormal ocular conditions.
The eye is highly complex, and the more I practised, the more I wanted to learn
For example, Munyal recently delivered an online CPD presentation with one attendee dialling in from a parked car and another based in Zimbabwe.
“The choices now are much greater than we had before,” he said.
Munyal is diplomatic when asked for his recommendations for courses that optometrists might consider completing post-qualification.
“I wouldn’t say to an optometrist ‘Do this or do that’ because I enjoy it. That is irrelevant They should find out what they enjoy. It starts with what rings your bell,” he said.
He shared that further learning has helped him to connect with like-minded people as well as making his job more enjoyable.
“If I hadn’t done these courses in the past, I probably would be doing a different job now. We sit in a room with a stranger with no windows and the door shut. It can be pretty boring if your job is simply to refract and sell glasses,” Munyal said.
The link between further learning and professional satisfaction is supported by the GOC registrant survey, with those who are intending to complete further qualifications more likely to satisfied in their role.
For Leicester optometrist, Azeem Awan, higher qualifications in glaucoma and independent prescribing have contributed to his professional development.
He has completed training in YAG laser under the supervision of a Moorfields ophthalmologist.
“I have learnt so much in all my training courses to make me a more confident practitioner,” he said.
Through a CUES IP contract, patients from the hospital are sent to Awan’s practice for assessment and treatment.
Awan also monitors stable glaucoma patients and recently purchased a YAG laser for his refractive surgery clinic.
He observed that if more optometrists complete further qualifications, it means that patients have a greater degree of choice about where to receive treatment.
“Once we have enough training then the future of a lot of emergency conditions and stable hospital patients can be managed in most optical practices,” he said.
Advertisement


Comments (0)
You must be logged in to join the discussion. Log in