- OT
- Life in practice
- Career development
- The student optometrists facing the challenges of the pandemic
COVID-Generation
The student optometrists facing the challenges of the pandemic
Over a year on from the first lockdown in the UK, OT is reflecting on the disruption current students and pre-registration optometrists have experienced, and the hurdles that remain

12 April 2021
When thinking back to university days, many people might reflect on academic work and placements, joining societies, or spending late nights with course mates in the students’ union – or perhaps cramming in the library. But since March 2020, the university experience has been turned upside down through lockdowns and restrictions brought about by the COVID-19 pandemic.
A time of changes and challenges
Reflecting on the effects of the pandemic, AOP policy adviser, Kathy Jones, told OT: “The last 12 months have been challenging for people in all parts of the optical sector, but we know the pandemic has been particularly disruptive for students and pre-reg trainees.”This disruption has affected several cohorts of pre-registration optometrists and undergraduates.
Luke McRoy-Jones, pre-registration optometrist, AOP council member and chair of the student committee, told OT: “I think that university staff deserve a lot of praise for their hard work, determination and commitment to the provision of optometry education and the development of online resources.”
Despite these efforts, McRoy-Jones suggested “real feelings of worry remain for current students.”
A key challenge for many universities and students has been moving content online.
William Holmes, University of Manchester senior lecturer and chair of the Optometry Schools Council, told OT: “To move into that kind of model requires a substantial amount of work.”
This has meant ensuring resources designed for in-person delivery are suitable for the remote learning environment, as well as arranging the logistics of delivering face-to-face sessions in a COVID-secure way.
The changes have also had a social impact, Holmes noted: “Most optometry courses are fairly tight-knit communities. There is a lot you can do with remote learning, but the corridor conversations and general socialisation isn’t able to happen.”
“There has been a slight sense of a moving target,” Holmes said, as restrictions have shifted, and the Government has changed plans in efforts to keep infection rates down – such as ending the term early for many students before Christmas.
With the vaccination roll-out and the roadmap out of lockdown ahead, there is a greater sense of certainty now, though Holmes acknowledged: “It’s fair to say that both staff and students probably feel more tired, and just like anyone else in the population, fatigued with everything that has to be complied with.”
Professor John Siderov, head of the department for optometry and vision sciences at the University of Huddersfield, commented that while many observers would agree the pandemic has brought “unprecedented challenges” to higher education, “for courses such as optometry, that incorporate significant clinical skills development as well as close patient interaction, the challenges are even greater.”
Safety has been central to the course’s approach through COVID-19, as well as adapting to virtual delivery. Staff have developed new course materials for online delivery, which have included finding innovative ways to teach clinical skills.
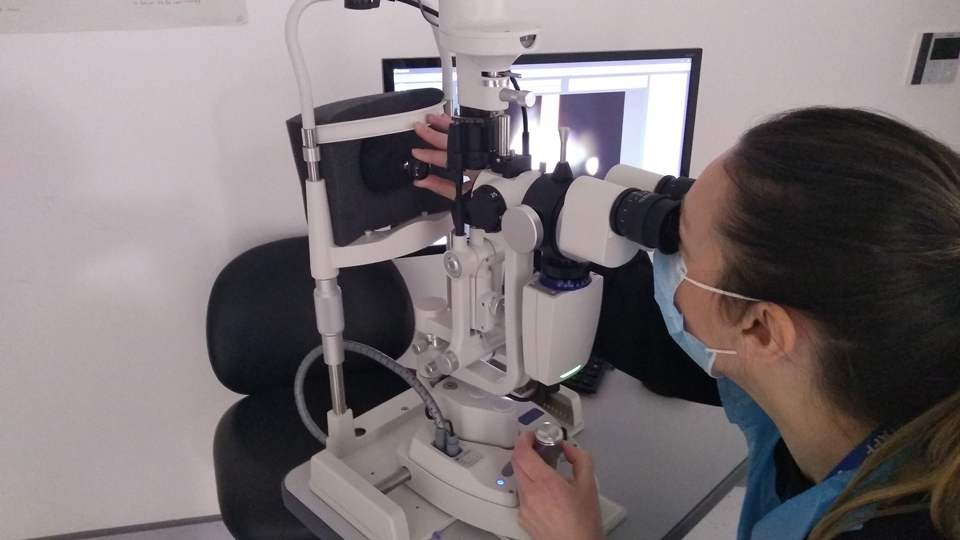
Siderov explained: “One example has been the development of a model eye using 3D-printing technology here at Huddersfield. The model is used for ophthalmoscopy training – pre-corneal lens and slit lamp – and can be used for retinoscopy skills work.”
The university also opened a new clinical teaching space in September 2020, creating more flexibility in scheduling classes.
Students have suggested that though challenging in some ways, the adaptations to teaching and assessments have had a positive side.
Recorded lectures can mean that students can watch them at a time of the day that suits them best, or can pause sessions to take more detailed notes, and many students described having helpful contact from their university and lecturers.
Indy Ghuman, second-year student at Aston University, told OT that the past year has seen greater innovation in teaching, with lecturers adapting teaching to be delivered in a more visual way online or with greater use of virtual patient simulators.
My experience: Saira Saleem
As a final year student, Ms Saleem expected to be making the most of her last year, but now: “When I attend university for clinics, it has become a ghost town.”
Though she feels learning virtually is not always as interactive as face-to-face teaching, the extra tutorials and case study scenarios have been helpful, as has the opportunity to see patients in visual impairment and binocular vision clinics virtually.
For more from Ms Saleem, look out for our student Q&A which will be live on the OT website in the coming weeks.
We are having to hone our primary care routines both in how to tailor, and how to do everything at the same time
Safely delivering practical sessions
One of the greatest changes to the university experience that students have highlighted has been the disruption to practical experience.While courses can continue practical sessions in-person where essential, lecturers have had to reduce student numbers to compensate for social distancing, and limit time on campus.
Ghuman told OT that it has felt “slightly worrying” for students not to be able to spend more time practising the techniques that “we will be conducting on a daily basis in our pre-reg and beyond.”
This has an impact on students’ confidence, he suggests, both for students moving into their final year and working with patients, and for third year students preparing for pre-registration.
One-year on from the first lockdown and with the use of personal protective equipment (PPE), lateral flow tests and COVID-secure operations, he questions whether there is scope to increase clinical training.
In order to support education providers to deliver teaching and training during the pandemic, last year, the General Optical Council (GOC) revised its Optometry Handbook and supervision policy to provide a more flexible and pragmatic approach.
Changes included further defining the minimum number of patient episodes that students must achieve in Stage 1, broadening the types of experience that can be considered, and reducing the total number of GOC Stage 2 patient episodes that must be achieved by 10%, while also removing categorised patient episode numbers.
The GOC also agreed to proposals whereby students with any outstanding Stage 1 competencies would be supported by the College of Optometrists to fulfil those in the early stages of their pre-registration placement.
This increased flexibility made it more feasible for courses to deliver the practical training that students needed. Mr Holmes said: “It means we are less focused on very specific arbitrary numbers and can be more focused on the rounded education experience.”
Holmes added: “I would argue that from a pedagogical perspective, whether or not COVID-19 had happened, it enhances what can count. It has always been my view that there is an element of narrowness to the current prescribed approach as its stands.”
My experience: Nkosi Yearwood
“As a result, we are having to hone our primary care routines both in how to tailor, and how to do everything at the same time,” Mr Yearwood shared. While an interesting skill to develop, he shared that this has felt more intense and stressful than previous years, adding: “You really feel the time pressure of limiting the patient’s exposure to the clinic.”
For more from Mr Yearwood, look out for our student Q&A which will be live on the OT website in the coming weeks.
Reflecting on students’ worries around practical experience, Holmes said: “I can understand students’ concerns,” but highlighted that at an undergraduate level, much can be gained from simulations and case studies, and cautioned against focusing too heavily on ‘real’ patient experience in university.
He explained that, in an environment with a real patient, there are certain situations that supervisors can’t allow to run their course: “For example, if you have a patient who is becoming angry or upset, a supervisor can’t let the student have that experience, but that can happen in a simulation.”
“I think, necessarily, there will be less ‘real’ patient experience at an undergraduate level, but I’m not altogether convinced that that is going to have quite the level of impact that some people are worried it might,” he concluded.
Similarly, for the transition between university and pre-registration, Holmes pointed out that the way many academic years operate might mean that students could, in normal years, have had their last clinical session in May, before starting their placement later in the year.
“I think there may be a potential bit of extra getting up to speed, but I think it is doable,” he added.
Operating in a COVID-safe way, Huddersfield has been delivering key clinical skills classes with smaller groups.
“Although we feel that we are offering a good clinical skills development for our students, we have had to limit other practical classes, in geometrical optics and visual perception,” Siderov said.
The steps taken by the optometry department have meant students in their second year have been able to continue with their clinical skills development, preparing them to be ready to examine ‘real’ patients in the second semester, while students in the first year have been offered similar practical skills times.
The course has introduced ‘practice’ sessions each week in semester two, enabling students in their assigned groups to gain more experience or catch-up if they have missed sessions, such as due to a need to self-isolate, and these are well-attended, Professor Siderov explained.
Community eye care practices are being called upon to support final year students
Securing experience in practice
In a normal year, students may expect to arrange work experience placements in various areas of optometry. Securing and delivering experience over the past year, however, has been one of the greatest difficulties for students and providers, explains Charlie Ball, head of higher education intelligence for the student and graduates careers organisation, Prospects at Jisc.Ball identifies twin issues to delivering work experience: “Students need to be able to get into the workplaces, but you also need people to assess and deliver effective assessments, at a very stressful time.”
Offering his own experience of these challenges, Ghuman told OT: “I was trying to organise a bit of hospital experience, because I’ve never had that experience before, but even just to get an afternoon or a few days has been near impossible.”
He added: “This is understandable given the circumstances, but in comparison to prior year groups, I will be applying for positions without having that reflection of what an optometrist in a hospital, or independent practice, does.”
Last year, Specsavers moved its work experience online as a ‘virtual store experience’ for students who had their summer placements postponed due to the pandemic, along with learning materials and resources.
While some practices will be able to offer in-store experience, this won’t be possible everywhere, explained Specsavers head of graduate recruitment and retention, Victoria Taylor. She added: “Given the changing landscape of the pandemic, we’ll repeat the same online summer placement offer that we had last year, to make sure there’s a provision for all students who want to join us.”
Speaking to OT of the challenges facing students as a result of the necessary COVID-19 infection control safety processes, David Quigley, chair of Optometry Scotland, highlighted that university colleagues had been doing “everything possible” to optimise clinical experience.
In support of this, Quigley said: “Community eye care practices are being called upon to support final year students by offering in-house clinical experience by way of observing eye examinations, clinical procedures and face-to-face examinations where possible.”
Additional measures discussed include remote tutorials and the possibility of utilising community practices or other clinical facilities on an out-of-hours basis. Quigley added that a gap analyses will be conducted, to evaluate the gap between the anticipated level of clinical experience and the reduced experience resulting from pandemic restrictions. Students will also be encouraged to work proactively with practices to volunteer support.
Moorfields Eye Hospital delivers a programme for undergraduate optometry students from City, University of London. This has been reduced this year, due to the limitations of social distancing on the numbers of people in the clinic.
Nathanael Anguige, principal optometrist and pre-reg supervisor, told OT: “In a typical year, the department will normally receive multiple requests from students to observe our clinics and to get a feel of how optometrists work at the hospital. Often, this helps them to decide whether or not they would like to apply for a pre-registration position either at Moorfields, or at another hospital.”
The department might also typically expect to see observers from around the world, but this has stopped as a result of the reduced capacity to deliver face-to-face teaching and observation, Anguige said. “We are hopeful this will resume once things settle with regards to the pandemic and restrictions are relaxed,” he explained.
Getting up to speed
“The OT skills guides offer practical video guidance on a range of clinical and dispensing topics and communication skills. They are aimed at students, pre-regs or qualified practitioners returning from a career break or who are training for a further qualification and need to revise something they haven’t done in a while.
“The presenters are university lecturers and expert practitioners. We explore the very basics of the sight test, such as setting up the trial frame, best sphere and cross cyl techniques, as well as more advanced techniques like applanation tonometry, using the slit lamp and binocular vision investigations. Video has its advantages over textbook learning, especially when covering something that requires a dynamic view, such as observing the vitreous to look for syneresis or Shafer’s sign.
“If you’re studying remotely, unable to get your hands on instruments and patients because of lockdown, these guides can help get you up-to-speed in preparation for the return to clinics.
“There are currently 32 guides in the OT education library; they can be found by filtering for ‘skills guides.’ If you have an idea for the next skills guide or if you have some expertise to share, please get in touch.”
This delay in qualification has significant impacts on these trainees, both financial… and also in terms of their wellbeing
Hurdles in the pre-registration journey
Changes and disruption to pre-registration optometrists who are already on, or beginning, their Scheme for Registration, have been among the most apparent impacts of the pandemic on the student population. In an OT poll in February 2021, 58% of pre-registration optometrists described their experience as ‘mostly negative,” with another 16% describing their experience as ‘somewhat negative.’ A further 19% said their year had been ‘both positive and negative.’
An AOP survey of pre-registration optometrists in autumn 2020, performed to understand the difficulties with placements, found that many trainees had been furloughed or taken on another role in the practice, while a small number were released from their position.
Speaking to OT, the AOP’s policy adviser, Jones, shared: “The hundreds of responses show us that most people who were in pre-reg placements at the start of the first lockdown, or had a placement secured, were in training but facing delays before they would qualify.”
The vast majority of those surveyed went back to their original placement, the AOP found, with an average short-term delay to their training of between three to six months.
Many trainees were due to sit the January OSCE, but the introduction of a third lockdown at the start of the year brought further disruption, as places were reduced due to a lack of examiner availability.
“This was a real blow to many of our members, who were expecting to complete the Scheme and join the register,” Jones shared. The AOP contacted the College of Optometrists to highlight these concerns, and were pleased extra days had been added in March to accommodate everyone.
It is anticipated that the delays to pre-registration optometrists could follow them through to qualifying.
McRoy-Jones suggested that the group most heavily affected has been the 2019 graduates, who saw assessments halted in March 2020 before resuming later in the year. He explained that “this group of trainees are now likely to qualify between April and July this year, rather than last summer as they would have been expecting to.”
“This delay in qualification has significant impacts on these trainees, both financial, having been earning a pre-registration optometrist salary for much longer than usual and with many having been away from home for longer, and also in terms of their wellbeing,” he continued.
For students preparing to join the Scheme for Registration this year or next, the availability of placements has been a key concern.
McRoy-Jones suggests that, with business confidence down and many candidates on the Scheme delayed, some supervisors may be reluctant to take on a pre-registration optometrist alongside the additional challenges of social distancing, PPE, and enhanced cleaning procedures.
To support pre-regs seeking placements, the AOP provides a free pre-reg register to match students with placements looking for a pre-reg.
“Looking ahead, we’ll be working with the rest of the sector on the challenge of ensuring that pre-reg placements are available for future cohorts of optometry graduates,” Jones shared.
The AOP’s employment team is also available to support members with employment law queries, including advising on pre-registration contracts, and the usual provisions the team sees included and enforced.
The Scheme for Registration 2021
“We know that this has been a difficult time, for both those who have recently graduated and those who have been moving through the Scheme, and we thank everyone for their patience,” Mr Shaw added. “We continue to work hard to ensure that trainees can progress to qualification as quickly and as safely as possible.”
There is not yet a start date for when the graduates of this year will begin their pre-registration training, Mr Shaw shared, adding that the College is in discussion with employers about when placements are likely to be available.
“This is dependent on current trainees’ progress through the Scheme,” Mr Shaw said, adding that while availability is set by employers, the College will continue to work with them to support the summer’s graduates.
“We are also awaiting a decision from the GOC as to whether the agreed COVID-19 scheme changes will be extended to the next cohort. This decision has to be made before the next cohort can start the Scheme,” he added.
Specsavers, a major provider of pre-registration placements and training, has been working to support the current cohort of pre-regs, and to establish placements for students due to graduate in the summer.
Taylor explained: “We've worked hard to make sure that all the optometry students who wanted to join our 2020–21 Pre-reg Academy could do so – and have actually offered more opportunities than we ever have. More stores are taking more than one graduate and we're also opening new stores.”
Specsavers confirmed to OT that in 2019/20, the business made 501 offers of placements, and for 2020–21 this increased to 550.
There has been some delay while the company prioritised supporting the 2020–21 cohort, Taylor acknowledged, but confirmed that Specsavers is now working with around 550 students to confirm pre-reg locations.
The company has also moved its joining process online, which now includes a video meeting for more than 700 students interested in the 2022 Pre-Reg Academy.
Speaking to Moorfields Eye Hospital, which would typically appoint four pre-registration optometrists each year to start in August, the hospital shared that as a result of the pandemic it has taken the decision to not appoint pre-regs for the 2021–22 year.
“By doing this, we hoped to increase the support and resources available to the 2019–20 cohort who were already employed at the hospital, as their year was turned upside down with cancelled assessments and reduced patient episodes until new guidance could be issued about how to proceed,” Nathaneal Anguige said.
This step has also created some flexibility to increase the length of the contract with the current pre-regs, who had their start dates delayed, in the event of any future changes as a result of the pandemic.
Commenting on the situation, Anguige said: “The pandemic is, and has been, an uncertain time for many, however the whole optometry team has rallied round the pre-registration optometrists, recognising that as junior members of staff, who may be locked down away from home, they may feel more vulnerable than others in the department.”
“We are hopeful that by August 2022, when our next cohort would be due to start, things will have settled back towards what we would consider a normal hospital pre-registration year,” he concluded.

Birmingham and Midland Eye Centre has also seen an impact on pre-registration optometrists.
Dr Waheeda Illahi, consultant optometrist and head of optometry services, and Dr Martin Cardall, senior specialist optometrist and co-ordinator of the hospital’s pre-reg and graduate optometrist placement, said that the placements allow students to develop a better understanding and awareness of patient pathways and what is needed in a good referral.
The professionals suggested: “In our opinion the one-to-one, face-to-face teaching sessions during hospital placements that the pre-registration optometrists are timetabled for with both ophthalmologists and experienced optometrists are precious and cannot easily be substituted.”
Considering how placements might need to adapt, the professionals suggested that aspects of hospital optometry teaching could be replaced by online tutorials or virtual live learning, to provide a mixture of face-to-face and online teaching. Illahi and Cardall added: “For some hospitals this may be difficult as the clinical workload for colleagues is not usually reduced during the students teaching session.”
Pre-registration HES packs with hints and tips on the subjects that students should read up on prior to attending their placement might also assist the student to be more prepared – and to have the confidence to ask more questions.
“We feel that even though there is tremendous pressure in the post COVID-19 era, these face-to-face hospital placements will continue to be of enormous benefit to pre-registration students,” Illahi and Cardall told OT, adding: “Considerable efforts are being made across the optometry profession to ensure that students are not disadvantaged in light of the lack of face-to-face patient interaction.”
In the meantime, they advised students and supervisors to contact as many hospitals as possible to identify potential placements as they may be limited.
“Optometry offers a wide variety of opportunities within the profession. It is possible to see a range of pathologies in your practice and we advise you to be proactive and use all the opportunities that are presented to you within your practice and hospital environment,” Illahi and Cardall shared, adding: “Stay focused and look towards a brighter future.”
Reflecting on the concerns around placement availability and the challenges facing pre-registration optometrists, McRoy-Jones told OT: “I remain hopeful that many placement providers see the value in having a pre-registration optometrist in the practice.
“Therefore, I am optimistic that placement availability and the job market could remain stable, particularly now that we have the vaccine roll-out and a greater understanding of the virus.”
Part two of OT’s COVID-Generation series will look at the impact the pandemic has had on student’s perception of the future of the profession, a growth in STEM subject applications, and considerations for the future of teaching and training in optometry.
Supporting students and pre-registration optometrists
Students and pre-reg members can use the AOP’s Pre-reg register to list their availability for a placement
OT’s education library hosts OT’s skills guides along with archived CET and CPD articles, covering a range of topic areas
The AOP’s employment team is available to support and advise AOP members on pre-registration contracts and employment law and can be contacted at [email protected].
OT would like to thank the following contributors:
- Kathy Jones, AOP policy adviser
- Luke McRoy-Jones, pre-registration optometrist, AOP council member and chair of the student committee
- William Holmes, University of Manchester senior lecturer and chair of the Optometry Schools Council
- Professor John Siderov, head of the department for optometry and vision sciences at the University of Huddersfield
- Indy Ghuman, second-year student at Aston University
- Saira Saleem, optometry student at City, University of London
- Nkosi Yearwood, third year student at Cardiff University and pre-registration councillor for Optometry Wales
- Charlie Ball, head of higher education intelligence for Prospects at Jisc
- Victoria Taylor, Specsavers head of graduate recruitment and retention
- David Quigley, chair of Optometry Scotland
- Nathanael Anguige, principal optometrist and pre-reg supervisor at Moorfields Eye Hospital
- Ceri Smith-Jaynes, optometrist and multimedia clinical editor for OT
- Alastair Shaw, head of assessment for the College of Optometrists
- Dr Waheeda Illahi, consultant optometrist and head of optometry services, and Dr Martin Cardall, senior specialist optometrist and co-ordinator of pre-reg and graduate optometrist placements at Birmingham and Midland Eye Centre.


Comments (0)
You must be logged in to join the discussion. Log in