- OT
- CPD and education
- The ABC of OCT

03 March 2019
Cast your mind back 15 years, when our mobile phones were used only to make calls and send messages. No emails, no internet, not even a camera. Advances in technology affect every aspect of our life and optometry is no exception.
Technology to help diagnose and monitor eye conditions has come a long way – in particular our ability to image the structures of the eye (see Figure 1).
Figure 1
OCT in action
OCT has been used for many years in hospital eye departments, but has become increasingly common in High Street practice. It can be thought of as the optical equivalent of ultrasound and works by shining certain wavelengths of light into the eye and measuring the amount reflected from the internal structures. It is most commonly used to image the retina; the light sensitive part of the eye, akin to the film in a camera. However, OCT can also be used to view other structures both at the front and back of the eye, such as the optic nerve head (which becomes damaged in glaucoma), and the cornea and iris.
Direct ophthalmoscopy is a staple technique which has been used for many years by optometrists to examine the eye. This involves getting very close to the eye with a bright light, which is quite invasive of personal space. Although techniques like this are still a necessary part of an eye examination, information they provide can be limited. Firstly, the view is restricted; only a small area of the retina can be seen at any one time (about 5°), and optometrists use movement to scan different parts of the retina to build up an overall mental picture of the inside of the eye. Secondly, because the optometrist uses only one of their eyes for this technique, depth perception is limited, making it more difficult to detect raised areas such as tumours.
Definitions
- Vitreous – the fluid that fills the main part of the eyeball
- Retina – the layered structure responsible for detecting light and converting it to a signal
- Choroid – the layer of blood vessels beneath the retina, provides oxygen and nutrients.
- Sclera – the ‘white of the eye,’ which keeps the shape of the eyeball
- Fovea – the central part of the retina with the highest resolution vision
- Optic nerve – transfers signals from the retina to the brain for processing
- Photoreceptor layer – the layer of light sensitive cells in the retina
- Pigment layer – the layer of pigment at the base of the retina; highly reflective so produces a bright band on the image.
Additionally, because it is performed on the slit lamp, it allows extra distance between the clinician and the patient, making it a less invasive experience. Although clinicians can reliably use these techniques to detect abnormalities, the results are recorded descriptively using words and/or drawings and are subjective. This means that they are open to interpretation, and different clinicians may describe features in different ways, making it difficult to monitor abnormalities over time.
Standard practice
Retinal photography (or fundus photography) is now commonplace in High Street practices. This can be used to capture colour images of the retina (typically covering 30–50°), which can be saved electronically and reviewed by clinicians. They can easily be compared between subsequent visits, making them excellent for monitoring abnormalities over time. However, they produce only two-dimensional images of a three-dimensional structure (like a normal photograph), which can make it difficult to assess the exact depth and extent of any abnormalities seen.
Figure 2
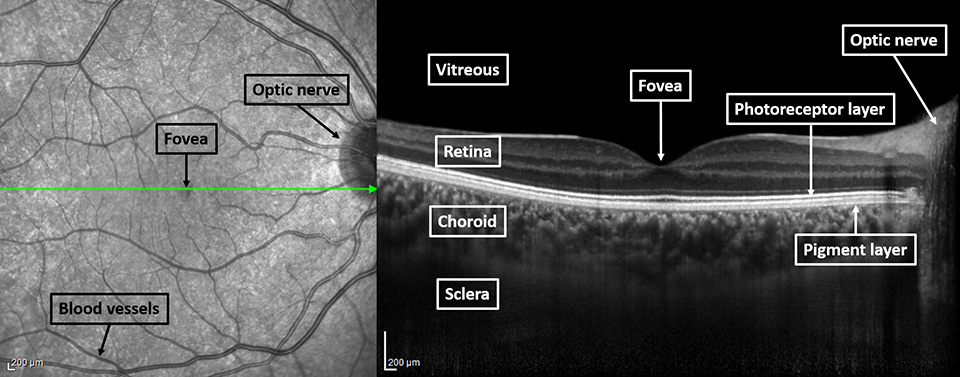
The retina is a complex layered structure made up of many different cell types, responsible for absorbing light and converting it to a signal to send to the visual areas of the brain for processing. Different eye conditions can affect different layers of the retina, and being able to assess which layers are affected in a patient is very useful – this is where OCT comes in. Unlike retinal photographs, OCT devices can be used to capture three-dimensional images of the retina within a matter of seconds, providing a wealth of information about the health of the eye. In particular, they can tell us information about the different layers of the retina (see Figure 2). Due to the cross-sectional view provided, OCT images enable clinicians to pinpoint the exact location of abnormalities seen on ophthalmoscopy or retinal photography, allowing accurate diagnosis and management of many eye conditions.
Other articles in this series
- 'Selling' the OCT concept to patients: Dr Neelam Patel's three points that every practice team should consider
- The OA's take: Zoe Harrison's views on developing your clinical skillset
- Fact from fiction: From visual fields to AMD, OT gets myth-busting
- Capturing the image: Taking the right steps at the right time
- The shape of things to come: OCT is evolving and OT explores the trends
- Patient outcomes: Dr Louise Terry on how OCT devices are helping to detect eye conditions
- My take on...OCT: Our experts' predictions on what is next for OCT.
Image credit: Heidelberg Engineering



Comments (0)
You must be logged in to join the discussion. Log in