- OT
- CPD and education
- Patient outcomes
Patient outcomes
Dr Louise Terry on how OCT devices are helping to detect eye conditions

10 March 2019
Optical coherence tomography (OCT) has changed the way many eye conditions are diagnosed and managed – it is now far easier to diagnose different conditions which may look similar on a retinal photograph or with ophthalmoscopy.
For example, macular degeneration has two main types: dry and wet (see Figure 1). The dry type is a gradual deterioration of the retinal cells at the macula, with a slow build-up of deposits seen beneath the retina, called drusen. This is a gradual change, and there is currently no treatment available.
Figure 1
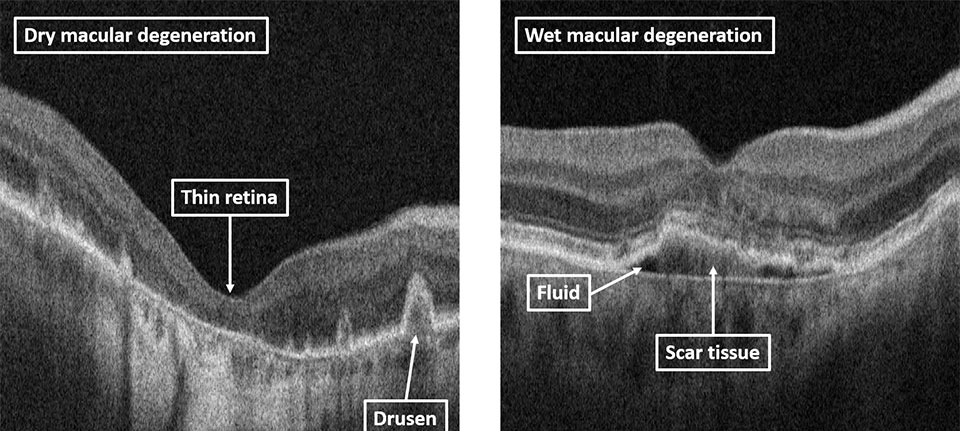
Wet macular degeneration is caused by leakage of new blood vessels at the macula, resulting in fluid build-up in the retina. This happens quickly and can be treated with injections to the eye, which prevent growth of the new vessels and allow the fluid to drain away. OCT imaging is used in hospital eye clinics to determine which patients have the wet type and therefore require prompt injections to treat it. This is a very quick and effective way to ensure treatment is given to those who would benefit from it and not given unnecessarily to those with the dry type.
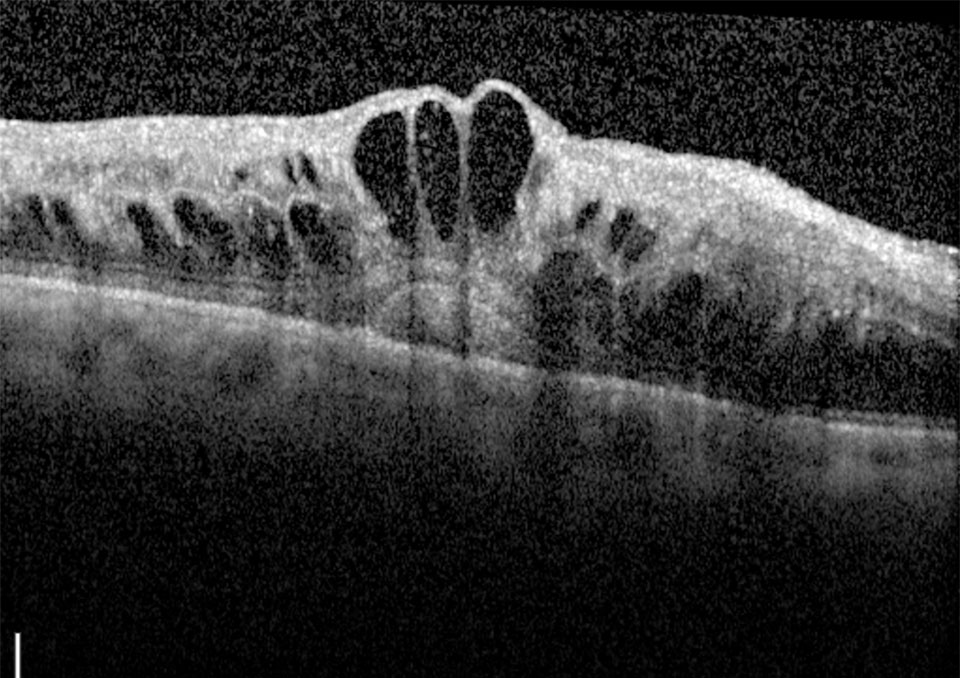
Figure 2
Quick and effective
Several other conditions of the macula can be detected using OCT imaging, including macular holes and macular oedema (swelling), which is common after cataract surgery, and in diabetic eye disease (see Figure 2). The optic nerve can also be scanned to detect signs of glaucoma, which is particularly useful for monitoring change over time and determining whether it is getting worse, requiring a change in treatment strategy.
Further forward in the eye, OCT can be used to assess the anterior chamber angle. This can become narrow and prevent the movement of fluid in the eye, resulting in a sudden increase in pressure known as angle closure glaucoma. Additionally, some OCT devices can be used to measure the thickness of the cornea and in contact lens fitting.
Other articles in this series
- 'Selling' the OCT concept to patients: Dr Neelam Patel's three points that every practice team should consider
- The OA's take: Zoe Harrison's views on developing your clinical skillset
- The ABC of OCT: Dr Louise Terry's back-to-basics guide to OCT
- Fact from fiction: From visual fields to AMD, OT gets myth-busting
- Capturing the image: Taking the right steps at the right time
- The shape of things to come: OCT is evolving and OT explores the trends
- My take on...OCT: Our experts' predictions on what is next for OCT.



Comments (0)
You must be logged in to join the discussion. Log in