- OT
- Professional support
- Health services
- The big questions
The cover story
The big questions
From sight test funding to mega mergers and the environmental impact of PPE, OT explores five issues facing the profession

19 June 2021
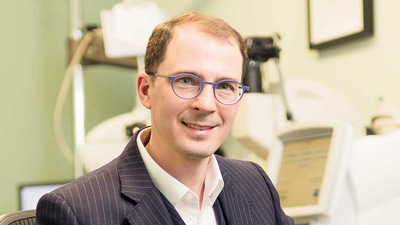
In March this year, optometrists working in Ontario, Canada came together for a virtual town hall meeting to address a question that has hung over each consulting room, each day, for decades. How can the profession achieve equitable funding of sight tests?
With close to nine in 10 Ontario optometrists in attendance, 96% voted in favour of a withdrawal of services from 1 September unless the Government agrees to make changes enabling a sustainable funding model.

Despite the slow pace of advancement, this the first time the optometrists of Ontario have proposed a withdrawal of services.
“For years, we’ve had times where a spark flares up and there is some hope of change and then it gets doused,” MacDonald said.
“Across the province within the profession there is a palpable sense that we are now at a point now where something is going to give,” he added.
Within Canada, decisions about the distribution of healthcare funding are made by the provincial Government.
Unlike other healthcare professions, such as nursing and medicine, optometrists do not have a formal negotiation process regarding how much they are reimbursed for performing Ontario Health Insurance Plan (OHIP) sight tests.
The fee for an OHIP sight test when MacDonald first started working was $39.15 and is now around $45 (£26.50).
MacDonald estimates that in Ontario, between 70% and 75% of patients seen by practices are funded through OHIP. Optometrists are unable to opt out of provincially-insured sight tests and patients are not permitted to pay out-of-pocket, or use private insurance to pay for provincially-insured services.
He described the level of provincial funding as a “losing proposition” where the care that professionals train for many years to deliver is the loss-leader.
“It is inarguable that it is inequitable. How can you expect a private practice, which is in essence a small business, to survive when they are losing money on every service they provide?” MacDonald emphasised.
The pandemic limited the number of patients that practices could see creating a challenging time for the optometry profession.
It is inarguable that it is inequitable
MacDonald noted that during the 11 weeks optometry practices were closed in Ontario, some optometrists began to wonder if they would ever be able to open their doors again.
“It pushed a lot of people to breaking point,” he said.
While funding is the tangible issue that the profession has focused on, MacDonald believes it is indicative of a lack of respect for the profession.
He added that successive governments from a variety of political persuasions have refused to engage with optometrists.
“We have always resisted the urge to withdraw services but there comes a point where you have no other cards to play,” MacDonald noted.
Firstly, an agreement that requires regular formal discussions between the association and the Ministry of Health, and secondly, the funding of OHIP sight tests on at least a cost-recovery basis.
“Our hope is that something changes long before 1 September and we can continue providing the services that we are trained to offer,” MacDonald emphasised.
MacDonald practises alongside his wife, who he met while studying to be an optometrist, at his practice in Waterloo, Canada.
He continues to work in the building where he started his first job – driving to the same address each working day for the past 29 years.
“It sounds cliché, but it really is the best job in the world. If I reach up into the cabinet above my desk, I still have the day sheet from my first day in practice. I still see some of the patients whose names are on that sheet,” MacDonald said.
Although funding has been an ever-present bugbear, MacDonald would not change his career choice.
“What trumps that 100 times over is that the patients we see value the care they get,” he emphasised.
Life-changing moments “each and every day”
Now he takes a call from OT in a room containing £150,000 worth of equipment to explain why his practice is parting with one constant in a world of evolving demands and technology – the General Ophthalmic Services (GOS) sight test.
“When I took over there was no thought of the possibility of not offering GOS tests, it was just what you did,” he shared.
“Everything we do has changed so much since then. The GOS fee has gone down in real terms over time, the IT demands have gone up, you have got to jump through so many more hoops. There comes a point where you stand back from it and think, ‘This is ridiculous. What am I doing?’,” Smith highlighted.
Smith will stop offering GOS sight tests at his practice from 1 August. His practice began offering an optional subscription model for receiving eye care six months ago, which has been positively received by patients.
Rather than being a decision based in finances, Smith said the outbreak of COVID-19 gave him the time to consider the big picture around how his practice was operating.
“It was more an ethical decision,” he emphasised.
“It feels honest, as a healthcare professional, to be working for a realistic fee,” Smith shared.
Fewer than one in 10 patients who come through the doors of Smith’s practice currently receive purely GOS services.
He noted that over time the gap between what his practice offers through GOS and the service provided through a private sight test has evolved to the point where there are few common elements –and where the optical regulator expects more from professionals than they are reimbursed for by the NHS.
When Smith started offering independent prescribing clinics, it highlighted the distortion that a low GOS fee creates in the market.
“You are charging a normal clinical fee for prescribing because there are no spectacle sales to make up the loss – suddenly your fees look massively disproportionate,” he observed.
It feels honest, as a healthcare professional, to be working for a realistic fee
Despite the long legacy of GOS at Smith’s practice, he does not feel anxious about his decision.
“I was massively, massively relieved. Once I made the decision to make that leap, it was like the scales falling from my eyes. I was thinking ‘Why didn’t I do this sooner?’,” he said.
Optometrist and chairman of BBR Optometry, Nicholas Rumney, shared that his practice continues to offer GOS even though he finds the level of reimbursement to be inadequate.
“We choose to work within the NHS because our area has nine enhanced care schemes enabled after years of persuasion and negotiation, and they won’t work with us if we leave the GOS,” he said.
Rumney emphasised that whether practices choose to remain with GOS or leave is dependant on a variety of factors.
“But it is not the responsibility of our profession to make up for deficiencies in government support,” he added.
Myers La Roche director, Dominic Watson, first helped a practice to go private seven years ago – a move which was considered unusual at the time.
The practice saw a short-term drop off in patient numbers and profit, before rebounding to normal levels within two years.
Watson shared that the practice owner had a better quality of life as a result of the switch.
“He had patients telling him ‘You look about 10 years younger’,” he said.
He observed that while there has been an increase in practices moving away from GOS, owners should give the move careful consideration.
“I can see some people potentially getting burned. I think it is going to be brilliant for many but it is not for everybody. It is understanding your patient base and your model,” he said.
Gordon Ilett took over the role of chair on the Optometric Fees Negotiating Committee (OFNC) in April. The national eye care body is responsible for negotiating the GOS fee with government.
When asked why he took on a role that involves tackling government inertia while also, at times, facing criticism from within the profession, Ilett said that he felt a sense of duty.
“What we must ensure is that those who are most vulnerable in society don’t lose out,” he said.
“I have yet to meet a critic who can come up with a good argument to say – ‘If you do this, you will get more money’,” Ilett said.
This year the OFNC confirmed that the Government would increase the GOS sight test for the first time since 2015 – from £21.31 to £21.71.
He believes that this year’s GOS increase signals a shift in approach from government towards the profession.What we must ensure is that those who are most vulnerable in society don’t lose out
“NHS England is waking up to the good that we do. They have recognised that they have fallen behind on the sight test fee as paid on inflation-adjusted ground alone, without taking into account the service improvements and developments in the scope of practice,” Ilett shared.
However, Ilett highlighted that the OFNC is aware that the increase is “nowhere near enough” to compensate practitioners for the time and resources they put into providing a service for the NHS.
In terms of his focus for the coming year, Ilett is planning to build on the work of his predecessor, Paul Carroll, who strengthened engagement with NHS England and the Department of Health during the course of the pandemic.
“We seem to have built relations to the point where we can have a dialogue about the symbiotic development of the eye care sector,” he said.
With the NHS facing burgeoning wait lists and an ageing population, optometrists are ideally placed to take some of the strain off secondary care by managing conditions within the community.
“As a nation I think the time is ripe to have a discussion about our funding for social care and for health care,” Ilett noted.
Ilett would like to see more research undertaken assessing the difference between the cost of offering a sight test in the UK and the level of reimbursement.
Understanding the impact of practices choosing not to offer GOS sight tests is also key, he observed.
“Will that disadvantage certain groups of the population? Will we end up with excellent services concentrated in affluent areas where people can afford to pay privately and will people in less affluent areas fail to be able to obtain even a basic examination?” Ilett shared.
COVID-19 has prompted a period of significant change on British High Streets.
Waves of shop closures prompted many independent practices to wonder what shape their local business hub would take as the UK emerges from the pandemic. How can optometry practices thrive amid an altered retail landscape?
Dominic Watson, of Myers La Roche, has recently published a report detailing his predictions for ‘megatrends’ that will shape the future of independent optics.
Turning to the steps that independent practices can take to remain resilient, Watson noted that tenants are in a good position to renegotiate their lease following the pandemic.
“There are massive opportunities to reduce fixed overheads on property,” he said.
A trend that Watson terms ‘islandification’ – where High Street businesses are marooned amid closed premises and shops that convert into residential units – means that footfall may not be the same as it was pre-pandemic.
“It is really important to either become a destination or look at moving,” Watson shared.
He shared that landlords are eager for new tenants, even in prime locations, which may help to sway practices considering a move.
“If you get it right, you can quickly claw back the cost of the refit and move,” he said.
Shifting working patterns present opportunities for independent practices to attract new customers into their practice who may have previously worked in an urban centre but are now seeking eye care closer to home.
Watson recommends that practices understand their catchment population, understand what their practice is offering and make sure the two elements are aligned.
“There is an opportunity to get new patients through the door by very much playing on the local,” he said.
Masks and other forms of personal protective equipment (PPE) have quickly become an essential part of practising as an optometrist during the pandemic.
As case numbers fall, will the use of PPE also decline? And if it remains, how can the environmental impact of PPE be minimised?
AOP head of clinical and regulatory, Henry Leonard, shared his view that PPE will continue in some form as we emerge from the pandemic.
“Despite the challenges inherent in examining patients whilst wearing PPE, and the extra time needed to follow more stringent infection prevention and control measures, many practitioners believe at least some of these measures are likely to remain in place for the foreseeable future,” he highlighted.
Leonard said that while the use of direct ophthalmoscopy has declined as a result of the pandemic, some procedures still involve getting close to the patient.
Examinations often take place in poorly ventilated consulting rooms and may last for a prolonged period of time – increasing the risk of transmission, not just of COVID-19, but other diseases such as seasonal flu.
“As healthcare professionals, we are mindful that these pathogens can still result in serious complications for older, more clinically vulnerable patients, who may have a range of underlying health issues,” he said.
Leonard noted that many practitioners are keen to wear at least a face mask going forward to provide themselves and their patients with greater protection.
“This should also result in fewer staff absences due to illness and help reduce the spread of diseases within the wider community,” he shared.

UK researchers from Royal Sussex County Hospital assessed the environmental impact of personal protective equipment in a paper published in the Journal of the Royal Society of Medicine in March this year.
Chantelle Rizan, Malcolm Reed and Mahmood F Bhutta estimated the environmental impact of personal protective equipment (PPE) distributed by NHS England in the first six months of the COVID-19 pandemic using a life cycle assessment.
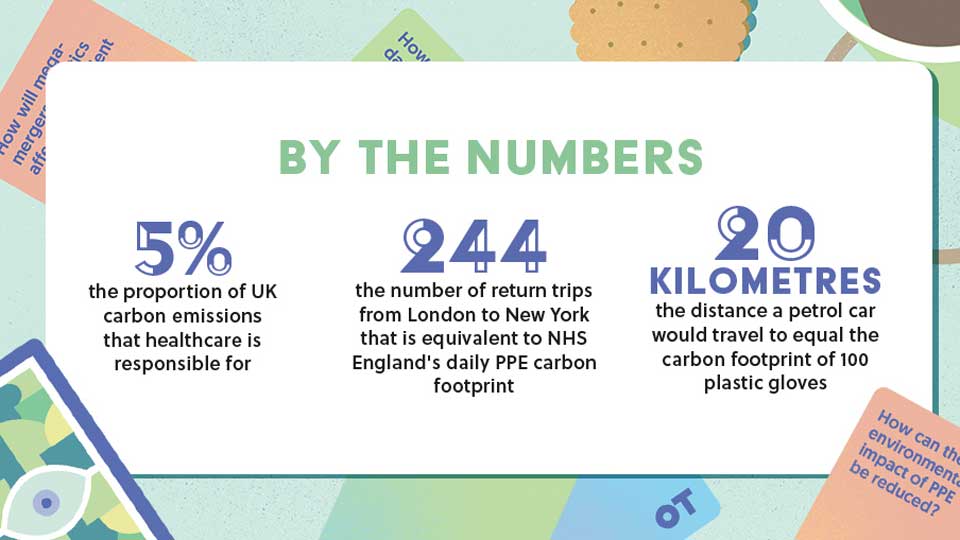
They calculated that the carbon footprint of the PPE distributed over the period was equivalent to 106,478 tonnes of carbon dioxide.
The authors note that, per day, this carbon footprint is equal to 244 return flights from London to New York.
Li Fang and Annie Pinder are both anaesthetists in the final stages of specialty training in the North West Deanery and became sustainability fellows in 2021.
With colleagues, they published a letter in the British Medical Journal in March discussing the need to mitigate the environmental impact of plastic PPE.
In response to questions from OT, Fang noted that single use PPE during the COVID-19 pandemic has added to the already significant impact of healthcare on the environment.
She shared that healthcare-related activities are responsible for around 5% of the UK’s total carbon emissions, as well as contributing to air pollution, water pollution and other ecological damage.
“Climate change and air pollution affect human health through multiple factors and worsen existing inequalities, so as clinicians we should seek to prevent further damage if we are to work towards a healthier population,” Fang emphasised.
“Whilst we acknowledge the many circumstances where PPE is required, we believe there are more sustainable alternatives to our current PPE repertoire,” she added.
Fang would like to see a reduction in single-use PPE, such as gloves, plastic aprons, face masks and plastic visors.
She noted that many instances of glove-wearing are unnecessary, with research showing that proper hand washing is equally effective in preventing transmission.
“Increased recycling and proper disposal of PPE would help to reduce the impact of plastics in landfill and incineration, and on our wildlife.
We would also like to see more research focussed on production of sustainable and re-useable PPE,” Fang shared.
When asked what steps clinicians can take, co-author, Annie Pinder, noted the importance of avoiding unnecessary PPE use.
She shared that every box of 100 gloves used has the equivalent carbon footprint of driving 20 kilometres in a standard petrol car.
“We think there is a role within all our professions to influence the procurement of equipment, opting for re-usable items, and ideally aiming to have supplies that are made domestically instead of abroad to eliminate the substantial emissions from international travel, especially by air freight,” Pinder highlighted.
Pinder shared that the pair are currently working on a project to calculate the carbon footprint of new PPE that has been designed for healthcare settings.
The ideal situation would be that all future design, manufacture and use of PPE considers sustainability as one of its priorities
Pinder and Fang will highlight areas of carbon cost and work with designers and developers to mitigate the impact where possible.
“The ideal situation would be that all future design, manufacture and use of PPE considers sustainability as one of its priorities,” Pinder emphasised.
When thinking about resources in primary care optometry, it is tempting to think about the latest pieces of equipment. But perhaps one of the most valuable resources is less tangible: the data that accrues every single time a sight test is performed in practice. How can this be harnessed to lend insight on the progression of disease and enhance future treatment options?
Research optometrist, Fiona Buckmaster, is working on a project to collect, classify and curate a retinal image repository from optical practices across Scotland.

“As an optometrist, I am really excited by this. I think it has potential to really impact the way that primary care optometry is delivered,” Buckmaster emphasised.
In Scotland, 1700 optometrists perform two million sight tests each year from around 900 optical practices.
Since 2006, routine sight tests using high-resolution retinal cameras have been funded by the NHS in Scotland.
“It means that there is now over a decade of rich longitudinal resources that are currently being stored in High Street practices,” Buckmaster said.
She shared that the data stored in optical practices has potential to lend insight not just into ocular disease, but systemic disease – with research suggesting that there can be retinal manifestations of conditions such as Parkinson’s, Alzheimer’s and cardiovascular disease.
“We want to know whether a routine eye examination could tell clinicians more about patients’ health,” Buckmaster shared.
The Scottish Collaborative Optometry-Ophthalmology Network eResearch (SCONe) project are currently undertaking a two-year feasibility study.
Optometrists in Scotland can register their interest in joining SCONe as pilot practices via email.
Those in Scotland and other areas of the UK are invited to complete an online survey to help researchers understand what images optometrists are capturing and the data management infrastructure they are using.
The research is funded by Chief Scientist Office, RS Macdonald Charitable Trust, The Royal College of Surgeons of Edinburgh, Sight Scotland Veterans, and Edinburgh & Lothians Health Foundation.
Harnessing data
Optometrist and AOP clinical director, Dr Peter Hampson, on how advancements in the use of data will affect optometry
Data in optometry has historically existed in discreet unconnected systems that makes comparison and follow up difficult. This can mean that optometrists are often unaware of what the patient’s status was at their last appointment, regardless of whether that appointment occurred in a primary care or secondary care setting. This can make it difficult to detect change and can lead to assumptions over the patient’s status and also unnecessary re-referral to secondary care.
Advancements in the use of data should help to tackle this challenge in a couple of ways. The first is to be able to more easily detect any change in a patient and the ability to quantitively monitor the progression of disease across a wider scope of environments. Data sharing across modes of care will reduce gaps in care, improve access and ultimately improve health outcomes for patients.
This should in turn allow quicker and more timely interventions as data trends become easier to spot and the inter-observer variability becomes less important. It also facilitates shared care and enables better collaboration between primary and secondary care.
The second, but linked point is that by increasing the volume of accessible data and the use of deep learning, our understanding and recognition of disease will also advance. One of the criticisms raised against current optical coherence technology (OCT) databases is that certain patients such as moderate to high myopes are underrepresented, leading to patients without disease being incorrectly flagged as outside of normal limits.
However, if we imagine a world where all of the data captured from OCTs across the UK, or wider was pooled and categorised, we could have a far greater understanding of what the “normal” patient actually looks like. This in turn should enable us to detect disease at an earlier stage and instigate treatment quicker, again this will improve outcomes for patients and facilitate the ambition of a greater amount of care delivered in primary care.
This is advantageous for patients, but also improves the role of clinicians and helps them to more fully utilise the extent of their training. For many this may also allow them to practise optometry in the way they envisaged when they embarked on their career.
In March, the European Commission approved the acquisition of GrandVision by EssilorLuxottica – with approval conditional on the divestment of some optical retail stores in Belgium, Italy and the Netherlands.
Three years after a merger between two global companies dominating the sale of lenses and frames respectively, what will the expansion into supplying directly to the consumer mean for independent optical practices in the UK?
Dr Cindy Tromans is president of the European Council of Optometry and Optics (ECOO), which represents optometrists and opticians working throughout Europe.
The concentration process that started at the industrial manufacturer level has now extended into the retail field
Tromans noted that vertical integration is expected to have a direct impact on these smaller players in the field.
“The effects of the Essilor and Luxottica merger in 2018 have been felt in the optical market already, so this new development gave rise to even greater concerns. For instance, it has the potential of limiting competitor access upstream and to provide restricted or delayed access to products downstream,” she said.
Tromans shared that ECOO members have highlighted concerns that as a result of the acquisition the company will be competing directly with independent practices and obtain a “significant competitive advantage.”
“This progressive market consolidation is a real risk for smaller players in their ability to compete and is expected to lead to higher prices for the customer in the medium to long-term,” she said.
The European Commission conditions in Belgium, Italy and the Netherlands involve divesting around 350 stores across the three countries.
While the restrictions are “a step in the right direction,” Tromans does not believe the conditions go far enough.
She also contends that the European Commission should have extended the conditions imposed within these nations to countries with similar market environments.
Tromans noted that a delay in access to innovative products is a risk for smaller market stakeholders.
“The concentration process that started at the industrial manufacturer level has now extended into the retail field. We think the next logical step will be an acquisition of a contact lens manufacturer and that the US market is a blue print for their strategy,” she observed.
The AOP is calling for members who experience a change in their relationship with EssilorLuxottica to share their experiences with its policy team via email.
Insight on closures, price changes and other information that provides a picture of the UK market is also welcome.
Advertisement


Comments (0)
You must be logged in to join the discussion. Log in