- OT
- Professional support
- Health services
- The waiting millions
The waiting millions
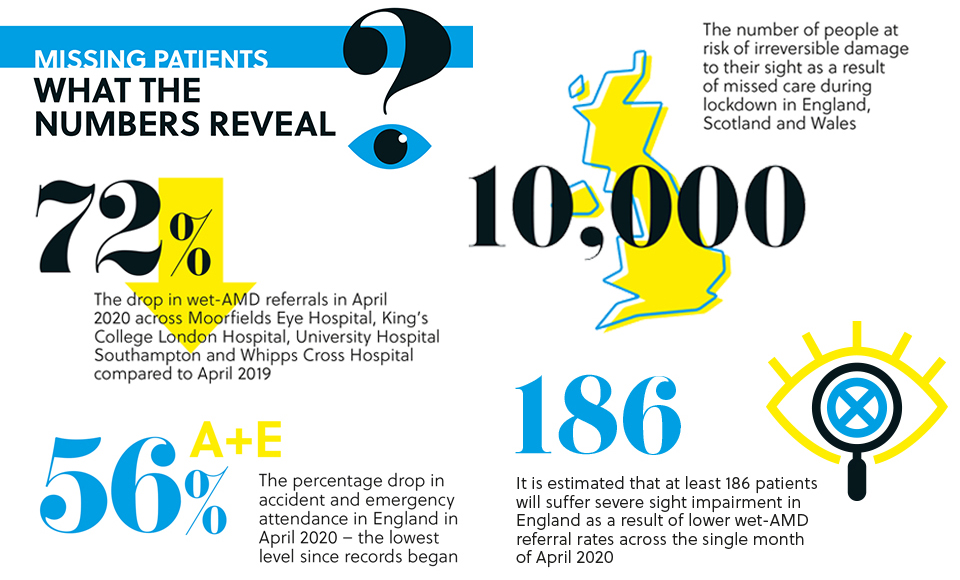
The NHS Confederation has estimated that the list of patients waiting for treatment could reach 10,000,000 by the end of the year. How can optometrists help to tackle a daunting backlog? OT investigates
19 August 2020
When she became worried about her left eye at the height of a global pandemic, Jennifer Slater turned to the same institution that has helped to keep her world in focus since she first attended Moorfields Eye Hospital more than six decades ago with Fuchs dystrophy.
But this time the appointment was a different experience. Instead of travelling to a fluorescently lit waiting room, Ms Slater’s appointment was a click rather than a tube journey away.
A clinician observed Ms Slater’s eye, asked her questions and emailed a prescription to her local pharmacist.
“I felt like I was in the clinic,” Ms Slater said.
“It made me feel so much better knowing someone could not only talk to me but see me.”
Ms Slater is one of 600 patients each week accessing Moorfields’ services through video appointments.
With social distancing requirements reducing the capacity of many clinics by close to half, remote care is becoming an increasingly important way of tackling a growing NHS backlog.
Attend Anywhere, the video consultation platform used by Moorfields, was used for around 1000 video consultations each day across the UK and Ireland before the outbreak of COVID-19.
Now 20,000 patients are seen daily through the technology – a number that is continuing to rise.
Rapid and radical change
Enhanced use of video consulting technology is just one way that Moorfields Eye Hospital has adapted to the challenges posed by the pandemic. Deputy head of optometry at Moorfields and AOP Councillor, Dr Vijay Anand, highlighted his desire for the momentum of change to continue as core services resume.
“Everybody knows there is pressure on the NHS, and ophthalmology is the highest outpatient specialty. I think it would be a real shame if we don’t change after learning what we are capable of,” Dr Anand added.
Analysis shared with the NHS Confederation estimates that the NHS wait list could reach 10,000,000 by the end of the year or possibly higher if there is a second wave of COVID-19 in the absence of a vaccine or effective treatments. Data published in October last year by NHS Digital reveals that ophthalmology recorded the highest number of annual outpatient appointments in 2019, with 7.8 million patients attending – 200,000 more appointments than the next closest specialty.
After lockdown was introduced, Dr Anand was part of a team that worked out how the skillset of 160 Moorfields optometrists and 20 dispensing opticians could be utilised within a radically and rapidly transformed model of providing eye care.
The usual network of 32 Moorfields Eye Hospital sites was reduced to eight, with some nursing and medical staff redeployed to aid the COVID-19 response.
Optometrists alternated between providing patient-facing and remote care on a weekly basis. They were profiled to assist in face-to-face clinics for high-risk patients within glaucoma, medical retina, accident and emergency and urgent care services.
During remote working shifts, optometrists staffed a pre-existing helpline that was “inundated” with calls following lockdown as many patients had routine appointments cancelled.
Optometrists were involved in taking around 5000 calls between April and the beginning of July, providing reassurance to patients and redirecting queries away from medical colleagues.
While many core optometry services were paused during lockdown, Dr Anand and his colleagues came up with innovative ways to continue to care for patients – albeit from a distance.
Optometrists provided 1300 low vision and 3000 contact lens consultations over the phone.
“People were grateful for that because they felt that they weren’t just lost in this system where they weren’t going to be seen again. It reassured them and identified those patients who we will bring back first as we open up services,” Dr Anand said.
Staff within the optometry department devised a home vision testing chart. Low vision patients were sent letter charts and pieces of string in various lengths in order to get a crude measurement of visual acuity. Optometrists would direct the patients on how to use this during telephone consultations and were able to reassure patients about any change in their visual acuity. Reading cards helped to judge what strength of magnifier a patient needed and these would then be posted out.
“A large proportion of the low vision patients were shielding due to their age or health conditions.
They weren’t able to have the usual support from relatives to aid with activities of daily living, such as reading letters. Continuing to provide a low vision service to these patients meant they were able to continue with their day-to-day lives,” Dr Anand shared.
Streamlined thinking
Within Moorfields alone, it is estimated that 40,000 glaucoma patients had their appointments cancelled during lockdown while 2000 cataract operations were either delayed or cancelled.
In order to address this backlog, the way that care is offered is changing across all sub-specialities.
Within glaucoma care, more patients will go through a virtual pathway. Dr Anand said that these reviews tended to be conducted by ophthalmologists before COVID-19, but more optometrists are now undergoing training to conduct virtual reviews.
Previously, between 80 to 90% of patients within the keratoconus monitoring clinic would be seen face-to-face. That could change to 30% of patients following the COVID-19 outbreak and lockdown, with the remainder of patients reviewed virtually.
“Patients would attend for a visual acuity measurement followed by corneal topography, anterior segment OCT and corneal hysteresis carried out by an optical assistant,” Dr Anand said.
“That information would be reviewed by an optometrist who would make the clinical decision on the stability of the patient's condition,” Dr Anand shared.
Cataract services could also become more streamlined, with a larger proportion of care offered remotely.
Dr Anand, who has worked within the cataract service for 16 years, highlighted that within a typical 25-minute face-to-face appointment the majority of time is spent detailing the risks and benefits of cataract surgery and a far smaller portion is spent conducting a physical examination of the eye.
“With the massive backlog of patients you could probably manage more patients with phone call consultations; establishing whether they want to have the surgery, how much of a risk they are in terms of COVID-19 and how much surgical risk there is, and discuss refractive planning before they even step into the hospital building,” he elaborated.
Dr Anand also believes there will be more opportunities to work with optometrists in the community to manage patients. He added that, following the outbreak of COVID-19, patients have become more forgiving of healthcare services working in different ways.
“In any sub-speciality there are lots of patients who have annual check ups. Many of these patients will be stable but still require monitoring due to the nature of their condition. Before the pandemic, many of these patients would still want to be seen in a face-to-face clinical setting. However, with new ways of working, and the involvement of community optometrists, many of these patients could be discharged to a different model of care,” Dr Anand observed.
“We could move these patients into primary care optometry with optometrists referring the patients back into secondary care if there is a change in the patient’s condition. That is the kind of thing that the profession as a whole should be striving for.”
Adapt and thrive
Initially, Dr Anand had hesitations about how staff would react to the rapid transformation of their working life.
How would colleagues adapt to homeworking – a concept that was largely alien to optometry in pre-COVID-19 times? Would they be comfortable working in unfamiliar roles? Would optometrists who needed to stay at home, because of health conditions or at-risk family members, feel isolated from the rest of their team?
However, Dr Anand emphasised that the optometrists working at Moorfields have been “absolutely brilliant.”
“They have really shown that you can put them in any situation and they adapt and thrive. They haven’t complained. Everybody has had the attitude, ‘That’s fine. I will do whatever you need me to do’,” Dr Anand said.
Asked by OT whether he has had a chance to pause and reflect as routine services resume, Dr Anand highlighted that there is still much work to be done.
“In six months, when we look back on this, we will say, ‘I can’t believe that we actually did that’,” he reflected. “It has been a completely unprecedented time.”
I saw four elderly patients with suspected wet-AMD in the first week after lockdown. Normally we see one every few months
During lockdown, Steve Wright kept his West Midlands independent optometry practice open for emergency appointments but did not receive many calls.
In the first week of returning to practice following the easing of restrictions, the optometrist and director of Malcolm Gray Optometrists saw as many patients with suspected macular disease as he would usually see in a year.
“I have seen four elderly patients with suspected wet-AMD. Normally, we see one every few months. When I referred these patients, the hospital co-ordinator told me that she had been inundated this week with wet-AMD referrals,” Mr Wright said.
He told OT that it appeared that some patients had delayed getting in touch with their optometrist during the lockdown period.
“Hopefully we are able to get these patients seen in time to save their vision, but I wonder how many people are out there with symptoms that need to be seen and managed before it’s too late,” Mr Wright emphasised.
A large proportion of the patients who attend the West Midlands practice, which has operated in the community for 40 years, are aged 60 and older.
Mr Wright highlighted that hesitations about contacting an optometrist for advice on eye health concerns could be leading to vision loss.
“The message needs to be that if anyone has symptoms with their vision, they should seek out professional advice over the telephone immediately and, if necessary, face-to-face. As a profession we are able to help patients maintain healthy vision and, in the event of symptoms affecting vision, we can help patients find the right solution,” he concluded.



Comments (0)
You must be logged in to join the discussion. Log in