- OT
- Industry
- Equipment and suppliers
- The role of OCT in supporting patients living with diabetes
Supplier insight
The role of OCT in supporting patients living with diabetes
OT looks at the value that OCT can provide for optometrists supporting patients with diabetes, and the importance of routine appointments alongside the national screening programme

09 October 2023
Figures show that 4.3 million people are living with a diagnosis of diabetes in the UK, while the charity estimates that an additional 850,000 people could be undiagnosed.
Routine eye examinations form a core part of managing the condition, and optical coherence tomography (OCT) can be an important tool in the optometrist’s belt for observing changes and providing reassurance and education.
A holistic view
5 million
people are estimated to be living with diabetes in the UK
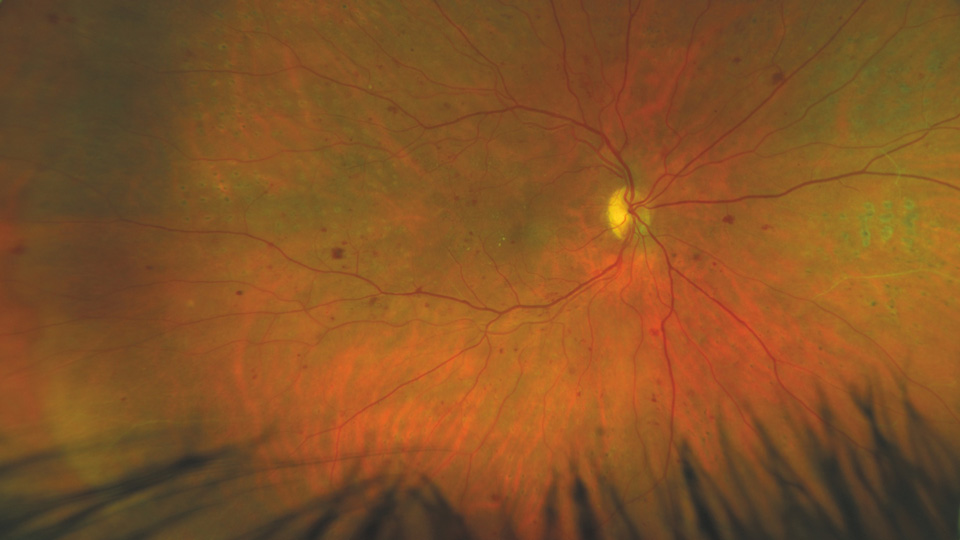
Sharon Ormonde, Optos sales director for Northern Europe, told OT: “Optometrists often tell us that patients who live with diabetes may decline enhanced tests (such as combined OCT and ultra-widefield (UWF) imaging) on the basis that they have already undergone their diabetic screening, assuming this includes a thorough assessment of eye health.”
Optometrists, meanwhile, will seek a more holistic view of eye health, Ormonde continued, and integrating OCT into routine sight testing in practice can help to provide that more complete picture.
“Optometrists frequently find themselves explaining this distinction to patients in their clinics,” she added.
As a potential aid supporting early diagnosis, OCT scans could provide a level of reassurance for patients.
Ormonde highlighted: “If a patient has a fundus image and an OCT, the optometrist can show them the back of the eye and explain what they are looking for. This offers all patients a peace of mind that they have had the most thorough review of their eye health possible (whether or not they are living with diabetes).”
Clinical confidence
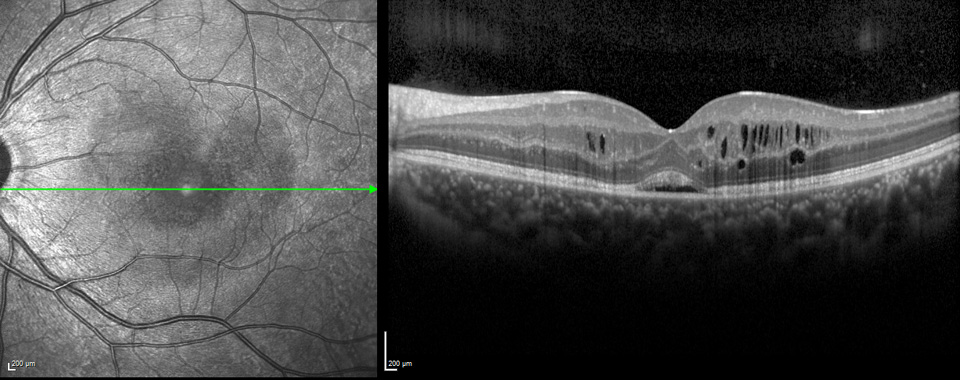
Claire Martin, head of strategy and marketing for ophthalmic diagnostics for Zeiss, emphasised that screening services “only take a basic visual acuity, without IOP or a slit lamp examination, and rarely include an OCT scan.”Modern OCT technology is able to diagnose diabetic macular oedema (DME) with a high level of accuracy, Martin shared, using “near micron accurate, three-dimensional measurements of the retina.”
For patients receiving a sight test in practice, Martin said: “All published studies have agreed that completing a separate OCT alongside colour fundus give the best results for early detection of diabetic retinopathy,” adding that 3D OCT scans provide the most accurate result for DME alongside the annual diabetic eye screening.
Using OCT in routine appointments can support the detection of other conditions, such as glaucoma or AMD. In addition, tools like the Cirrus 6000 offer a wellbeing report with an overview of the retina and RNFL, which could be taken to the next screening.
An educational tool
Emmeline Webb, clinical sales specialist for Heidelberg Engineering, said: “Having an OCT available during a routine sight test would benefit the patient by offering early reassurance or diagnosis regarding any ophthalmic concerns caused by diabetes.“Images could also be used as a visual tool for the patient, helping them to understand how their diabetes can be affecting them as an individual.”
A variety of factors, such as poor glycaemic control and the length of time that an individual has had diabetes, can affect an individual’s care.
"Offering more information and advice to the patient could allow them to feel more confident regarding the management of their diabetes, which could help to improve their overall mental health and wellbeing,” Webb added.
Using fundus photography and OCT images as a teaching tool can support a patient’s knowledge of their condition, and “this also helps them understand how they are being affected directly, as they can see visual changes.
Shared care
Manufacturers identified the ongoing move to see more patient care delivered closer to home.“There is a drive to shift patient care increasingly towards community settings,” Ormonde said.
Initiatives vary across healthcare systems, but technology can provide the information needed to help detect changes earlier, enable earlier interventions, and improve patient outcomes.
“The goal is very much to preserve a patient’s vision for as long as possible; while detecting changes, the emphasis is on identifying them at the earliest stages to enable proactive intervention,” she added.
Zeiss’ Martin noted that patients can fall between the screening service and hospital eye service: “not needing treatment but needing more advanced and accurate images taken than two-dimensional colour fundus.”
“Community optometry with OCT diagnostics will be able to test and review patients that need repeatable OCT to confirm whether the patient’s diabetic retinopathy is stable or improving with the ability to quickly refer patients back to the hospital eye services when needed,” Martin said.
Community optometry can help to reduce false positive referrals for diabetic eye screening to the hospital eye service, the spokesperson added, as patients flagged with significant makers could undertake an OCT in a community setting to review DME.
Elizabeth Woodstock, clinical sales specialist for Heidelberg Engineering, also reflected on the increasing interest in shared care, commenting: “Building a strong relationship between primary and secondary care can be a beneficial solution for both parties, ultimately improving the accessibility of timely care for patients with various eye disease.”
“Moving forward, I anticipate that the role of OCT imagine will continue to expand in community optometry, with an OCT device being an invaluable asset to any practice,” she concluded.
Communicating the value of OCT
Martin, Zeiss: “OCT offers the more accurate diagnosis for DME than standard colour fundus eye screening. OCT can also test for multiple other eye conditions that standard eye screening cannot detect.
“All studies have shown that early detection for DME is essential for the best outcome. Diabetic patients who attend annual eye screening should take the opportunity to have an OCT at the optician as this will give the earliest and most accurate diagnosis for diabetic retinopathy.”
Webb, Heidelberg Engineering: “Using patient images, I would explain to them what pathology was present and how that pathology would impact the patient’s care pathway – I.e. whether they would be referred routinely, urgently, or discharged.
“I have found that some patients would have very little understanding of the condition, the possible effects of retinopathy, or the importance of attending regular appointments, even though they would have been diagnosed with the condition for several years.”
Woodstock, Heidelberg Engineering: “In recent years, the presence of optical coherence tomography imaging devices in optometry practices has been rapidly increasing. It has proven to be a valuable tool in the management of various eye conditions and provides the optometrist with more information about their patient’s eyes than ever before.
“With such thorough eye tests, knowing the optometrist is monitoring eye health with such precision promotes a patient’s trust and loyalty to a practice.”
Ormonde, Optos: “Independent optometrists play a key role in patient education; for example, explaining what is or is not included in current screening procedures. If a patient has a fundus image and an OCT, the optometrist can show them the back of the eye and explain what they are looking for.
“This offers all patients a peace of mind that they have had the most thorough review of their eye health possible – whether or not they are living with diabetes.”
OT asked: what role can OCT play in identifying signs or symptoms of diabetes-related conditions?
The diabetic eye screening service first launched in England 20 years ago and is available once a year for individuals with diabetes who are over the age of 12.
Manufacturers discussed the potential benefits that OCT could have for early diagnosis.
Zeiss’ Martin explained that the two-dimensional mydriatic colour fundus photography used in the screening relies on three significant markers to predict diabetic macular oedema (DME):
- Exudates within one disc diameter of the fovea
- Circinate within two disc diameter of the fovea
- Visual acuity 6/12 or worse with microaneurysms or haemorrhages within one disc diameter of the fovea.
Martin indicated that these significant markers produce a high number of false positives when used to diagnose DME: “27% of those with macular exudates and 17% with haemorrhages or microaneurysms had macular thickening, resulting in around three out of four patients not having DME.”
In addition, some patients may have DME but none of the significant markers from standard two-dimensional colour fundus technology, the spokesperson shared.
Heidelberg Engineering’s Webb agreed that utilising OCT results could help to reduce the number of unnecessary referrals into the hospital eye service, and suggested that the current use of 2D retinal fundus photography can make it difficult to assess swelling of the retina.
“Recent studies have shown how OCT can differentiate between features of pre-proliferative retinopathy and proliferative retinopathy, which could change a routine referral to an urgent referral,” they said.
Ormonde described how Optos has collaborated on diabetic retinopathy studies, including with the Joslin Diabetes Centre at Harvard University, which found that integrating Monaco OCT into a diabetic screening programme that utilised ultra-widefield images improved the detection of diabetic retinopathy and macular pathology by 62%.
“Most notably, cases which would have been overlooked when relying solely on UWF were identified through OCT,” Ormonde shared, adding that this indicates the value of using both OCT and UWF in conjunction.


Comments (0)
You must be logged in to join the discussion. Log in