- OT
- Industry
- Equipment and suppliers
- Striking gold in myopia management
Supplier insight
Striking gold in myopia management
With axial length being a key outcome measure in myopia management, OT heard from manufacturers designing instruments to support data capture, and sought out available tools

08 July 2023
Guidance from professional optical bodies suggests that axial length is the optimal measurement to take when assessing levels of myopia and the effects of myopia management solutions.
A focus on axial length
Danielle Lee, Topcon Healthcare’s clinical affairs manager for the UK and Ireland, explained that there has been a definite increase in demand for devices that can measure axial length since the release of new guidance from the College of Optometrists in 2022.Don’t forget
OT has released the 2023 Myopia Guide, with the latest insights, tips and guidance on incorporating myopia management into practice.
Darren Taylor, qualified optometrist for more than 20 years and product training manager at Essilor Instruments UK, suggested that: “The industry is now exploding with talk of myopia management.”
Considering the growing levels of awareness of myopia management in the industry, and among the public, Taylor said: “I can see similarities to what happened with OCT in the market a few years ago: the more patients and parents enquire about myopia management, and the more practitioners talk about it, the more it will become the norm.”
Myopia Expert 700
Taylor suggested practices are keen to gather more data to enhance eye examinations and offer more to patients.
Essilor’s Myopia Expert 700 features corneal topography with integrated optical biometer for axial length measurement. It can also offer pupillometry and fluorescein assessment. Data capture can be delegated if required.
The Myopia Care software also supports practitioners with communication, allowing for axial length data from the Myopia Expert 700 and refraction data to be combined with patient questionnaires and myopia risk factors. Data is presented in graphs and percentile growth charts and can be turned into a PDF report for patients and guardians to take home with any additional information.
Discussing the importance of communicating this data, Taylor said: “If a patient is to start down the route of myopia management, it could be six, eight, maybe 10 years, that they need to be on that pathway. It is very important to have a way to keep them engaged throughout that time.”
For parents and guardians in particular, Taylor noted: “For most people, it’s fairly easy to understand where we are now, but parents always want to know where are we likely to be heading in the future?”
Considering investing in a device to support myopia management?
Darren Taylor’s key questions for practices to reflect on:
- How many children are on my database? More importantly, how many do I want on the database? Having more children visiting the practice has to be a good thing, as it secures your patients for the future
- Where will the new device be located in practice and who is going to operate it? The practitioner’s time is a very expensive commodity in the practice, so delegation could be key
- Is any more learning or knowledge needed before we can confidently have a myopia conversation with parents and patients? The practices where it tends to work best are where any practice team member can have at least a top line conversation with parents
- Is having a new device better than what I currently offer? Having something that is going to make a difference and add value for the patient is key
- Will the new service enhancements provide an in-practice experience which is better than before, and better than your competitors?
Topcon’s MYAH
Lee described a change in the optical landscape since the MYAH was released in Europe in 2020, suggesting that, with the prevalence of myopia expected to significantly increase, demand will continue to rise, adding: “We’ve got more practitioners offering myopia clinics, and the public are becoming much more aware.”The MYAH device offers corneal topography, keratoconus screening and pupillometry, along with capturing axial length measurements, and the measurement process can be delegated. The device also incorporates a suite of dry eye assessment tools.
The device can be used to assess risk and start myopia conversations, monitor axial length and compare measurements with growth curves, drawing on the Erasmus University dataset.
Lee explained that this “huge” European-specific dataset has been gathered over a number of years, assessing patient populations. Incorporating this data into normative growth curves provides an indication of where the patient is in comparison to what is expected, in the same way a parent might look at height and weight charts for their children.
“From a clinician’s point of view, it enables those conversations to be had earlier, as we can see how the prescription and axial length are changing over time, what to then expect in later life, and the risk of the patient becoming myopic or a high myope,” Lee said, adding that once an intervention has been started, “we can utilise that data to monitor treatment efficacy and compliance.”
Lee suggested this provides a multifactorial approach, as the device provides a lot of data that can be utilised in different ways, “depending on what part of the journey the patients are at.”
This data can also be exported into a variety of reports, including a report for the patient.
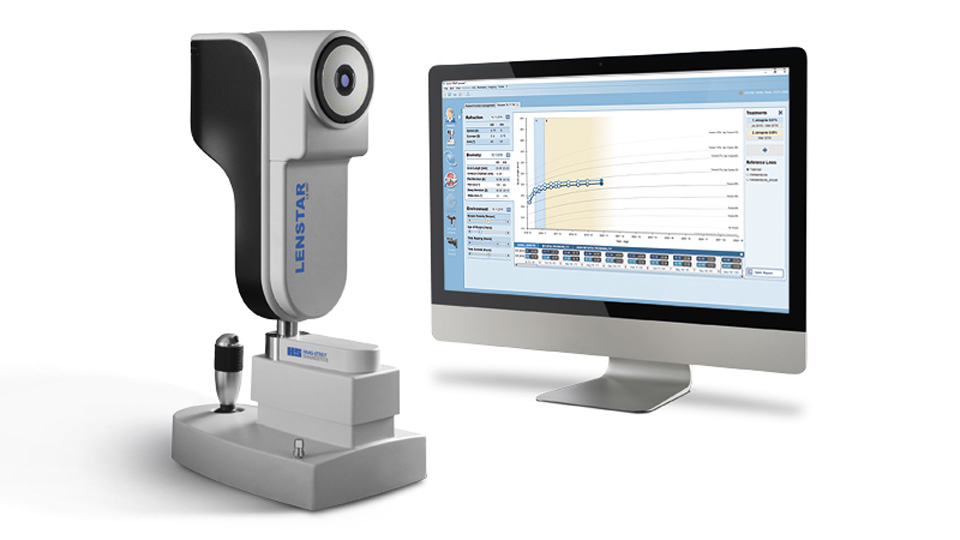
Lenstar Myopia
Haag-Streit launched the optical biometer, the Lenstar Myopia, in the first quarter of 2021 and has seen demand “increase dramatically” in the last year, Grahame Wood, national sales manager at Haag-Streit UK, said.“As awareness of effective myopia management continues to grow, an increasing number of practices will see the need to adopt technology to aid in their clinical decision making and patient/parent education,” he explained.
The Lenstar Myopia system is made up of the Lenstar 900 optical biometer with corresponding EyeSuite Myopia software. The biometer enables axial length measurement, as well as pupillometry, vitreous chamber depth, central corneal thickness and keratometry.
The software allows for previously-collected data from refraction and measurement devices to be imported, and environmental factors to be defined.
Designed to help facilitate the consultation and education of patients and parents, the software also utilises axial length growth curves from the Erasmus University Medical Center.
Features include displays for tracking treatment interventions, showing refraction curves, axial length measurement and environmental factors, such as outside time versus screen time and parental history of myopia.
Wood explained: “The system has a great report that explains in an educational, easy-to-read way, a description of myopia, the risk factors if left untreated, treatment regimens, and how the patient is responding.”
Haag-Streit plans to launch an additional smart software add-on to the Lenstar Myopia. Wood explained: “The AMMC (Age Matched Myopia Control) module developed by Dr Kaymak looks at speed of axial length growth of the patient over time and categorises the speed of growth using a simple traffic light system that is easy for patients and parents to understand.”
“This will aid practitioners on when to intervene, for example, if growth is too fast. In addition, it shows the effectiveness of treatments over time on slowing the rate of growth,” he added.
Starting out
The right time to invest in a device for measuring and monitoring axial length will be individual to each practice.
Manufacturers emphasised the importance of education for practices new to myopia management, or who may not feel ready to invest in a biometer.
Taylor said: “Keep up to date with the most recent research, and understand what the different myopia management solutions will do, how they work, and how they are aiming to reduce abnormal axial length growth.”
He suggested that practitioners should be able to have a conversation with a patient about myopia, and recommended that, if they are in a practice that doesn’t yet offer any myopia management pathways, to know where to point the patient for more information.
Lee encouraged practitioners to make the most of resources available on websites such as Myopia Focus, through CPD, or provided by the manufacturers of devices, ophthalmic lenses or contact lenses.
She said: “There is a huge amount of people out there willing to support – some of them have been doing myopia control clinics for a number of years and are willing to share their experiences. There’s great value in asking others for their experiences and learning from them.”
A tool for myopia management
New companies are also seeking to offer innovative solutions to support practices in discussing myopia with patients.
Established by Professors James Loughman and Ian Flitcroft, Ocumetra’s mEYEguide is a global web-based platform designed to “streamline” conversations around myopia.
The tool can be used to create personalised reports for the patient, that their parent or guardian can take away by simply scanning a QR code on their mobile phone.
As part of the package, practitioners also gain access to the mEYEgauge, an axial length estimator that uses routine optometric measures and patient variables, with an average error of less than 0.25mm.
Corrina McElduff, director of professional affairs at Ocumetra, explained that the introduction of the estimator tool came from an understanding that “for someone first starting out with myopia management, it would be unlikely for them to be able to invest in a biometer from the start.”
The tool incorporates key variables including patient gender, prescription, age and K-readings and provides an estimated adult axial length, vision impairment index, and how this compares to an emmetrope.
“This helps to understand the clinical context of axial length in practice,” she said, considering “what axial length is normal for an individual patient, and what degree of change you might expect over the next year or so, with or without treatment.”
The software has more than 1 million datapoints incorporated into the tool, as well as hundreds of scientific papers, with an Asian and a Western database separated into two normative reference databases.
Investing in instruments
It isn’t only the practices at the forefront of myopia management who are investing in devices, with Lee sharing: “We’re seeing practitioners that have never done myopia control before that are getting on board with it and using a device like this as their introduction to it, to help them along the way with that learning.”Taylor identified that a common thread between the practices who have made the investment of a device was a desire to offer more enhanced services: “The main aspect is practices don’t want patients to slip through their net, they want to keep things in-house as much as possible.”
There are multiple pathways for purchasing equipment, he added, that don’t necessarily require “signing a cheque there and then.”
Lee also recommended considering what would suit the clinic workflow, and any additional functionality a device might offer.
“You want something that’s easy to use, either in the practitioner’s room or something that can be delegated to optical assistants, depending on that clinic workflow, and something that is easy to talk through with patients,” she said.
For those looking into this kind of instrument, Wood also recommended: “If you are already conducting myopia management, or wishing to introduce this, then investment in this type of technology will certainly add value to your practice, both from a clinical and patient loyalty perspective.”
Estimating axial length
AOP guidance recognises that while measuring axial length change is optimal for myopia management, “these measurements are not widely used in mainstream clinical practice at present.”
The Brien Holden Vision Institute offers a free Myopia Calculator which shows the range of myopia management options and demonstrates the possible benefits over time of starting to treat myopia progression.
The BHVI shared with OT that, in the 12 months between the end of March 2022 and start of April 2023, the calculator received more than 100,000 page views – an increase of 9% on the previous year, and a 17% increase in unique page views.
The International Myopia Institute also provides free online resources for myopia management, such as the IMI Facts and Findings Infographic, designed as a “chairside” reference and communication tool, and has recently released a series of white papers around myopia management in practice.
Free tools also include those developed by Ulster University such as the PreMO Risk Indicator, Axial Length Growth Charts and a table to support estimating axial length.
In brief: advanced technology in myopia management
Throughout June and July, OT is exploring the role that artificial intelligence (AI) could play in optometry. Read the feature here.
As part of this theme, OT asked manufacturers for their quick takes on how myopia management could evolve in the future, and the role AI could play.
Taylor shared that, as our understanding of how the eye grows, and what influences this, increases: “We’re better placed to offer data for monitoring and management. The more we understand, the more we can offer in the future, and the more we can do about it.”
“I envisage that axial length will become a routine part of examining children. It will just be part of what we do when a child comes in for an eye test. I fully expect parents to expect it as the norm in the not too distant future,” he added.
Thinking more broadly about the potential for myopia management in the future, experts pointed to discussions around screening and insights for management.
Lee shared: “There seems to be some thought that there may be benefits in terms of predicting risk and treatment efficacy, and potentially to offer personalised treatment plans in the future.”
She suggested that, in the future, there may be solutions that help to determine which patients are likely to be the most responsive to certain treatments, or likely to progress the fastest, but emphasised that discussion was speculative at present.
Corrina McElduff, at Ocumetra, expects to see a shift towards discussing myopia in terms of millimetres, rather than solely dioptres, and anticipates seeing enhanced tools that will serve multifunctions.
Considering AI, she suggested: “I think we’ll see more personalised eye care. Optimised treatment selection, monitoring and refinement, which eventually with AI, can begin to become increasingly specific as we acquire more data on what available treatment options can do or achieve, depending on the profile of the patient.”
McElduff highlighted that, in myopia management, not all patients at the same level of refraction or axial length develop eye disease or vision loss, and so AI could help optometrists make predictions of those patients most at risk, and most in need of a timely intervention.
“We would definitely say that the future is exciting for myopia management, and I think we’ll certainly see technology being at the forefront of that,” she added.
While AI might seem to be at an earlier stage in myopia, manufacturers all highlighted that there is much discussion and opportunity for AI in other areas, such as OCT or glaucoma.
Advertisement


Comments (0)
You must be logged in to join the discussion. Log in