Myopia management in clinical practice
Evidence-based guidance on the management of myopia in practice
By 2050, it is predicted that half of the world’s population will have myopia, with 10% projected to have high myopia.1 Risk factors for myopia include parental history, environmental factors, and being of East Asian ethnic origin.2 The presence of myopia increases the risk of several ocular pathologies, including myopic maculopathy, glaucoma, cataract and retinal detachment.3 While those with high levels of refractive error are at greatest risk, even low myopes have an increased likelihood of developing these conditions over their lifetime.3
In the UK, the prevalence of myopia in children has more than doubled in the last half a century and is manifesting at a younger age,4 leading to a greater proportion of children with high levels of refractive error.
Given the rising prevalence and trend for earlier onset of myopia, there has been growing interest to adopt strategies to help mitigate for the risks of progressive myopia and the development of ocular disease in later life. Other benefits from retaining a lower level of refractive error include better uncorrected and corrected visual acuity, improved vision-related quality of life, reduced dependence on correction,5 improved outcomes from refractive surgery,6 and a higher likelihood of meeting occupational vision standards. In addition, patients can benefit from improved comfort and cosmetic appearance of spectacle appliances if the refractive error is retained at a low level.
There are a range of licensed interventions available in the UK, which aim to slow axial growth and myopia progression,7 as well as evidence-based lifestyle modifications that can help to delay the onset, and potentially progression, of myopia.8-11
The uptake of myopia management interventions in mainstream clinical practice is becoming more widespread. As such, you should keep your knowledge up to date, with a good understanding of available options, including the benefits and limitations, in order to offer appropriate advice to patients. In addition, it is important for members of the practice team who are involved in the patient journey to understand that the decision to recommend a myopia management intervention should be directed by the optometrist on a case-by-case basis. A range of clinical scenarios are provided later, which outline potential management approaches in each case.
If you, or the setting you are working in, do not offer myopia management interventions, then you should be able to establish which practitioners in the local area offer these services so you can direct patients if needed.
Lifestyle interventions
Time outdoors
Spending time outdoors can help to prevent and delay the onset of myopia development in children.8,11 The mechanism for this remains unclear but is likely to be multifactorial. If the onset of myopia can be delayed, this is likely to reduce the magnitude of the refractive error and reduce the risk of developing ocular comorbidity in later life.12 With this in mind, you should advise children at risk of myopia, for instance, those with a parental history of myopia and/or a low level of hyperopia for their age, to spend more time outdoors where possible. Based on current evidence, the advice should be to encourage children at risk of myopia to spend between 80 to 120 minutes of accumulative time outdoors per day.7 Time outdoors may also slow the progression of refractive error in existing myopes but the evidence for this is less certain.8,11
Near activities
More time spent in education is a known risk factor for myopia, and although the mechanism remains unclear, this may be due to time spent on near tasks.2 Despite this, current evidence does not strongly indicate that reducing time on near activities prevents the development or progression of myopia.9 Nevertheless, reducing non-essential time on near tasks, such as digital devices, by taking regular breaks, along with spending more time outdoors, offers a balanced approach that can be easily implemented.
Optical interventions
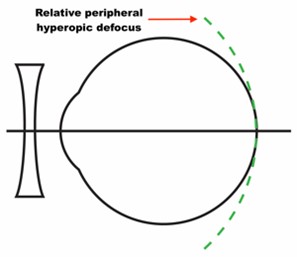
Single vision correction of myopia results in the eye being exposed to relative peripheral hyperopic defocus which is thought to drive axial growth (see Figure 1).7
It was once considered that undercorrection of myopia might slow its progression. The current evidence shows no benefit from undercorrection, with some studies demonstrating an increase in progression with this approach.13 With this in mind, regular sight tests to ensure that myopes are fully corrected is advised.
The mainstay of optical interventions for myopia management is to impose myopic defocus (see Figure 2) with the aim of slowing down axial growth and subsequent myopic progression.7
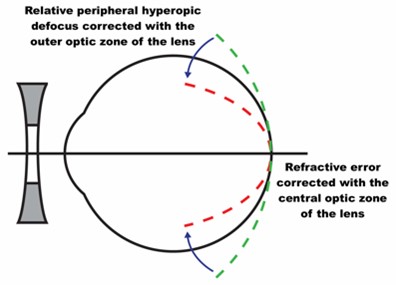
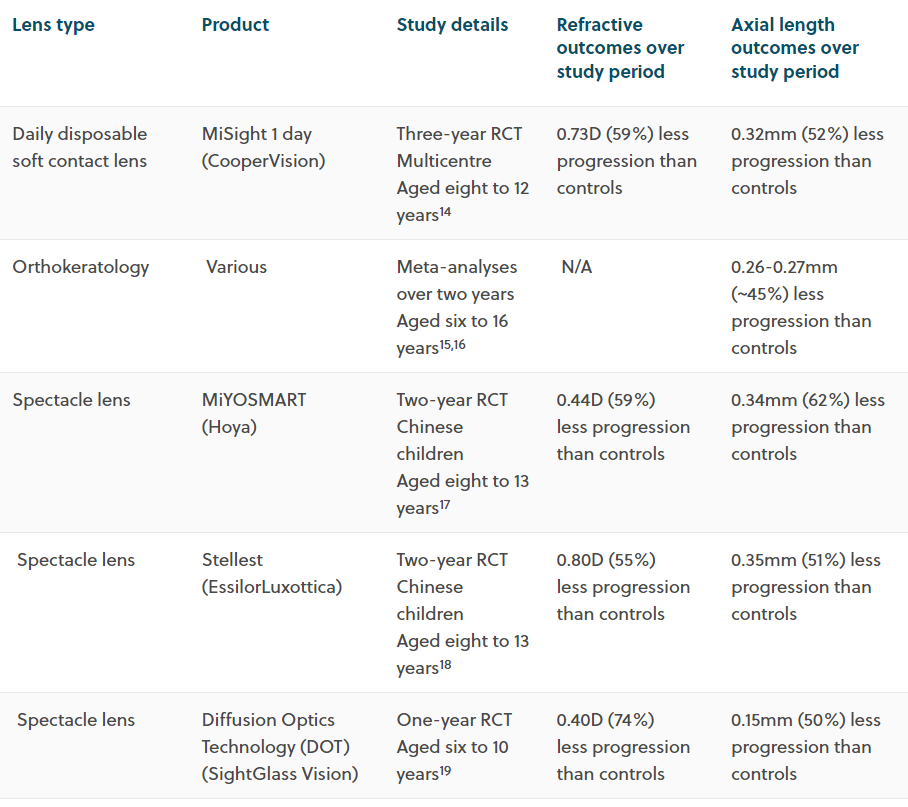
Table 1 provides a summary of outcomes from randomised controlled trials (RCTs) and meta-analyses for myopia management spectacle and contact lens options currently available in the UK.14-18 In short, all of these trials report similar outcomes for the average reduction in myopia progression and slowing of axial growth (compared to no intervention) over a one to three-year period. Evidence shows that these optical interventions deliver a visual performance that is comparable to single vision lenses.14,17
Safety of contact lens wear in children
The literature shows that contact lens wear for children, including orthokeratology, is considered safe, provided that appropriate advice on safe wear is followed to reduce the risk of infection.20 Reassuringly, the incidence of corneal infiltrative events in children is no higher than in adults, and in the youngest age range of eight to 11 years, it may be markedly lower.21
Off-label use of contact lenses for myopia management
In cases where a patient’s refractive error falls outside of the available parameters for a specific myopia management product, a suitable alternative, for example, a multifocal contact lens,22 can be considered as long as an evidence-based approach is taken to justify its use.
Other interventions
Atropine
Atropine is used in various parts of the world for myopia management but is not currently licensed for this purpose in the UK. At 1% concentration, atropine is effective at slowing myopia progression but has unacceptable side effects, including mydriasis, accommodative impairment and risk of allergic reaction, and is also associated with a significant rebound effect upon cessation of treatment.7 While lower doses of atropine in concentrations ranging from 0.01% and 0.05% have been shown to be clinically useful, the optimum dose, frequency and duration of treatment is yet to be determined.7
Repeated low-level red-light therapy (RLRL)
RLRL is an emerging intervention for myopia management, where the patient is exposed to short durations of low-level red light (typically three minutes, twice per day, separated by at least four hours, five days per week) using a table-top device, intended for use at home. RLRL has been used to treat amblyopia in China for decades and anecdotal findings of increased choroidal thickness and stabilisation of axial elongation in those receiving this treatment has led to interest in using this approach for myopia management. At present, research outcomes come from studies of relatively short duration and only extend to cohorts in China.23-26 The safety of accumulative exposure to RLRL for myopia management over the longer-term is currently unknown. However, a 2023 case report27 highlighted retinal damage occurring in a child after five months of RLRL, with partial recovery upon cessation of treatment.
Furthermore, a paper published in January 2024 has highlighted that the output from some RLRL devices could put the retina at risk of photochemical and thermal damage, underlining the need for caution when using this therapy in clinical practice.28 Given the conclusions of this work, practitioners should ensure regular follow-up of children undergoing this treatment and adopt a low tolerance for risk.
Practitioners offering RLRL therapy should ensure they keep their knowledge up to date in this evolving area of clinical practice and remain vigilant for unexpected findings. It is recommended that practitioners establish baseline measures of retinal function prior to treatment, such as visual acuity, monocular colour vision, en face fundus images and OCT scans, and repeat these regularly to enable comparisons to be made throughout the treatment period.
Case scenarios
The young, progressing myope
Seven years of age. Sits close to TV. Eyes ‘normal’ at previous sight test 12 months ago. Father myopic.
Refraction:
R -1.00DS
L -1.00DS
An evidence-based risk indicator29 can be used to guide management based upon the patient’s age and refractive progression. Note that as the data used to develop this risk indicator is primarily derived from a study in Northern Ireland,4 it is best suited for use with primary school children of white ethnicity living in the UK.
Given the age of onset and change in refractive error over the past 12 months, this child is at high risk of myopia progression. An evidence-based discussion about myopia management interventions would be appropriate here, covering the following points:
- Outline in broad terms why it is necessary to try and slow down myopia progression due to potential ocular health implications. The basis of this discussion should be balanced and in the context of absolute risk of ocular comorbidity that may arise in later life
- Advise on lifestyle modifications including time outdoors and limiting non-essential near tasks where possible
- Discuss the types of optical interventions that are currently available and their relative merits and limitations
- Indicate how long the intervention might be needed for, which could be well into the teenage years when risk of progression is lower
- Stress that individual outcomes cannot be predicted, and that the expectation is to slow down, rather than stop or reverse myopia progression.
Practitioners can use a myopia calculator30 to establish average anticipated outcomes with and without a range of interventions over the long-term. These projections can help to avoid the potential for over-promising and manage patient expectations in line with the latest evidence.
The nature of the discussion may take place across several visits and delivered in line with the patient’s and parents’ level of understanding.
Due to the age of myopia onset and refractive change over one year, a six-month review would be appropriate in this case.29
The older, stable myope
15 years old. No family history of myopia. First Rx prescribed two years ago:
R -1.25DS
L -1.00DS
Refraction today:
R -1.50DS
L -1.25DS
This patient has a relatively late onset, low magnitude of myopia which is progressing slowly. The following approach could be taken in this case:
- Advise a two-year recall unless the patient develops symptoms in the meantime
- Although the refractive error is stable, advice on lifestyle modifications would still be appropriate
- A single vision intervention would be suitable here and can be justified accordingly on the records, along with clear instructions from the optometrist to guide the dispensing process.
The child at risk of myopia
Six years of age. Attending for his first routine sight test. Both parents myopic. Cycloplegic refraction:
R +0.50DS
L +0.50DS
Keratometry:
R 7.62 along 90, 7.68 along 180
L 7.68 along 100, 7.72 along 10
Keratometry readings can be used to help predict future risk of myopia in the absence of biometry.29
This child has a high risk of developing myopia by the age of 10 years due to a low level of hyperopia for his age and a strong parental history of myopia, as determined using an evidence-based risk indicator.29
In terms of advice to the family:
- A one-year recall would be appropriate, unless the patient develops symptoms in the meantime
- Spending time outdoors and limiting time on non-essential near tasks could help to delay the onset of myopia.
Measuring success
Being able to directly measure axial length change over time is the optimal method for assessing outcomes; however, these measurements are not widely used in mainstream clinical practice at present.31 Consistent methods of refraction should be used between visits to ensure comparable clinical data.31 Cycloplegic autorefraction allows for repeatable, objective assessment to review change between baseline measures and follow-up visits.
Axial length growth charts32 can also be used to see how an individual patient’s measurements compare to age-expected norms and allow monitoring over time to help predict the risk of myopia, and in cases where an intervention is used, to give an indication of its impact.
Record keeping and consent
When offering myopia management interventions, it is important that informed consent is undertaken, with appropriate details noted on the records, in accordance with GOC Standards of Practice 3 and 8, respectively.33
The AOP has produced an information leaflet,34 approved by the Plain English Campaign, which includes a detachable consent form to be completed by the patient’s parent or legal guardian.
The leaflet is designed to be used by a practitioner to reinforce advice given to the patient and their parent or legal guardian during the examination. If you are recommending myopia management interventions for a child or young person you should explain what myopia and myopia management is before providing them with this leaflet.
Once the patient’s parent or legal guardian has read the leaflet, and you are confident that they understand the risks of myopia, and potential benefits and limitations of current myopia management interventions, you should ask them to complete the consent form at the end of the leaflet. A copy of the consent form should be kept with the patient's records.
What we don’t know
Although the myopia management evidence base continues to evolve at pace, uncertainty remains in some areas:
- At this moment, it is not possible to predict an individual’s response to a given intervention
- While there is some encouraging evidence emerging to demonstrate what happens when an intervention is withdrawn,35 a greater understanding of long-term outcomes, including the potential for rebound effects, across a range of different interventions is required
- Although the primary aim of myopia management is to reduce the lifetime risk of ocular comorbidity, the impact of slowing axial elongation upon long-term clinical outcomes is unknown at present
References
- Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016 11:00025-7
- Morgan IG, Wu P-C, Ostrin LA, et al. IMI Risk factors for myopia. Invest Ophthalmol Vis Sci 2021 62(5):3
- Haarman AE, Enthoven CA, Tideman JWL, et al. The complications of myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci 2020 61(4):49
- McCullough SJ, O’Donoghue L, Saunders KJ. Six year refractive change among white children and young adults: evidence for significant increase in myopia among white UK children. PloS One 2016 11(1):e0146332
- Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019 96(6):463-465
- Gomel N, Negari S, Frucht-Pery J, et al. Predictive factors for efficacy and safety in refractive surgery for myopia. PLoS One 2018 13(12):e0208608
- Jonas JB, Ang M, Cho P, et al. IMI prevention of myopia and its progression. Invest Ophthalmol Vis Sci 2021 62(5):6
- Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta‐analysis and systematic review. Acta Ophthalmol 2017 95(6):551-566
- Foreman J, Salim AT, Praveen A, et al. Association between digital smart device use and myopia: a systematic review and meta-analysis. Lancet Digit Health 2021 3(12):e806-e818
- Gajjar S, Ostrin LA. A systematic review of near work and myopia: measurement, relationships, mechanisms and clinical corollaries. Acta Ophthalmol 2022 100(4):376-387
- Dhakal R, Shah R, Huntjens B, et al. Time spent outdoors as an intervention for myopia prevention and control in children: an overview of systematic reviews. Ophthal Physiol Opt 2022 42(3):545-558
- Németh J, Tapasztó B, Aclimandos WA, et al. Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur J Ophthalmol 2021 31(3):853-883
- Logan NS, Wolffsohn JS. Role of un-correction, under-correction and over-correction of myopia as a strategy for slowing myopic progression. Clin Exp Optom 2020 103:133-137
- Chamberlain P, Peixoto-de-Matos SC, Logan NS, et al. A 3-year randomized clinical trial of MiSight lenses for myopia control. Optom Vis Sci 2019 96(8):556-567
- Si JK, Tang K, Bi HS, et al. Orthokeratology for myopia control: a meta-analysis. Optom Vis Sci 2015 92(3):252-257
- Sun Y, Xu F, Zhang T, et al. Orthokeratology to control myopia progression: a meta-analysis. PloS One 2015 10(4):e0124535
- Lam CSY, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol 2020 104(3):363-368
- Bao J, Huang Y, Li X, et al. Spectacle Lenses With Aspherical Lenslets for Myopia Control vs Single-Vision Spectacle Lenses: A Randomized Clinical Trial. JAMA Ophthalmol 2022 140(5):472-478
- Rappon J, Chung C, Young G, et al. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomised controlled, efficacy and safety study (CYPRESS). Br J Ophthalmol 2022 bjophthalmol-2021-321005
- Prousali E, Haidich AB, Fontalis A, et al. Efficacy and safety of interventions to control myopia progression in children: an overview of systematic reviews and meta-analyses. BMC Ophthalmol 2019 19(1):106
- Bullimore MA. The safety of soft contact lenses in children. Optom Vis Sci 2017 94(6):638-646
- Walline JJ, Walker MK, Mutti DO, et al. Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The BLINK Randomized Clinical Trial. JAMA 2020 324(6):571-580
- Chen Y, Xiong R, Chen X, et al. Efficacy Comparison of Repeated Low-Level Red Light and Low-Dose Atropine for Myopia Control: A Randomized Controlled Trial. Transl Vis Sci Technol 2022 11(10):33
- Dong J, Zhu Z, Xu H, et al. Myopia Control Effect of Repeated Low-Level Red-Light Therapy in Chinese Children: A Randomized, Double-Blind, Controlled Clinical Trial. Ophthalmology 2023 130(2):198-204
- Jiang Y, Zhu Z, Tan X, et al. Effect of Repeated Low-Level Red-Light Therapy for Myopia Control in Children: A Multicenter Randomized Controlled Trial. Ophthalmology 2022 129(5):509-519
- Xiong R, Zhu Z, Jiang Y, et al. Longitudinal Changes and Predictive Value of Choroidal Thickness for Myopia Control after Repeated Low-Level Red-Light Therapy. Ophthalmology 2022 S0161-6420(22)00780-1
- Liu H, Yang Y, Guo J, et al. Retinal Damage After Repeated Low-level Red-Light Laser Exposure. JAMA Ophthalmol 2023 141(7):693–695
- Ostrin LA, Schill AW. Red light instruments for myopia exceed safety limits. Ophthalmic Physiol Opt 2024 Jan 5
- www.ulster.ac.uk/__data/assets/pdf_file/0011/826184/PreMO-risk-indicator-for-website.pdf [Accessed 10/01/2023]
- www.bhvi.org/myopia-calculator-resources/ [Accessed 10/01/2023]
- Gifford KL, Richdale KR, Kang P, et al. IMI – Clinical Management Guidelines Report. Invest Ophthalmol Vis Sci 2019 60(3):M184-M203
- www.ulster.ac.uk/__data/assets/pdf_file/0009/826182/Axial-Length-Growth-Charts.pdf [Accessed 10/01/2023]
- www.optical.org/optomanddostandards/ [Accessed 10/01/2023]
- www.aop.org.uk/advice-and-support/business/resources-for-your-practice/myopia-management-consent-for-treating-a-child [Accessed 10/01/2023]
- Hammond D, Arumugam B, Bradley A, et al. Prior myopia control effects retained upon cessation of dual-focus soft contact lens wear. Invest Ophthalmol Vis Sci 2022 63(7):245-A0099

