Tackling the hospital outpatient backlog in eye care
A national strategy for eye care is essential to tackle the challenges in ophthalmology
The challenge
An ageing population
The ageing population is having a significant impact on the NHS backlog in the UK. As people live longer, they are increasingly likely to have more complex and chronic health conditions that require ongoing care and treatment. This includes an increase in the number of hospital admissions, outpatient appointments, and A&E attendances. The growing demand increases waiting times and provides a poorer experience for everyone who requires NHS services.
Additionally, the ageing population is also more likely to require social care support. As social care services have faced cuts and reduced funding in recent years, this has further increased the pressure on NHS resources.
The COVID-19 pandemic
The COVID-19 pandemic has also had a significant impact on the NHS backlog, with many non-urgent appointments and procedures being postponed or cancelled to free up resources to enable the NHS to deal with the pandemic. As a result, the backlog of patients waiting for treatment has grown even larger.
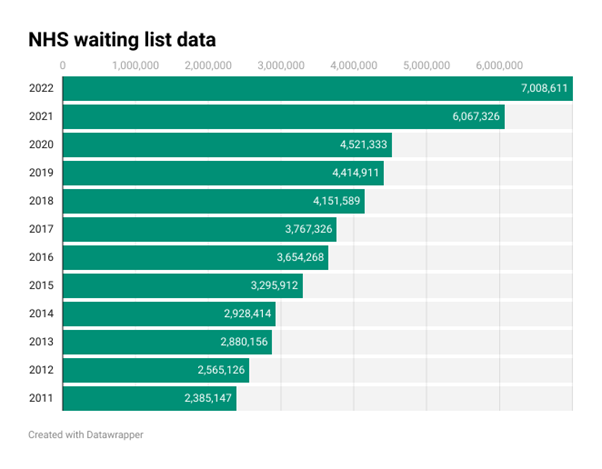
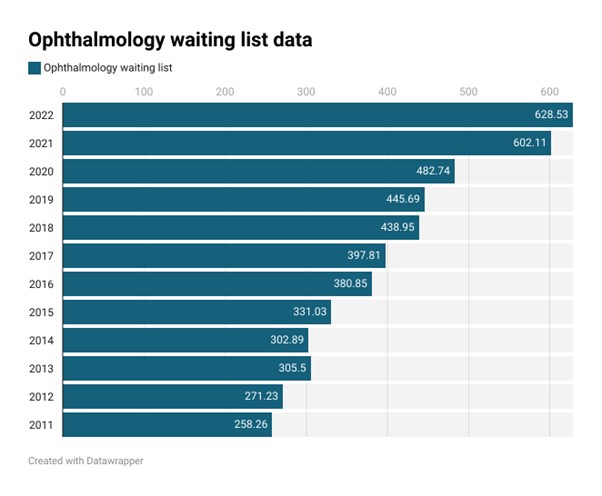
Increasing NHS waiting lists
In December 2011 there were just under 2.4m people on waiting lists in England, but according to official statistics published by NHS England, in December 2022 there were over 7m people on NHS waiting lists in England.1 Of those, around 630,000 were waiting for ophthalmology appointments, in comparison to around 260,000 in 2011.2 This is perhaps unsurprising as ophthalmology is the busiest outpatient speciality; in 2022 around 7.5m ophthalmology patient episodes occurred in England alone. By 2030 this activity level is projected to rise to around 9m patient episodes, fuelled by the chronicity of the conditions that this speciality deals with.2
The lack of ophthalmologists
Public Health England estimates that there are around 2.5 consultant ophthalmologists per 100,000 population in comparison to the recommended level of 3.5 consultant ophthalmologists per 100,000 population. To achieve a level of 3 consultant ophthalmologists per 100,000, would require an additional 250 FTE consultant ophthalmologists. The Royal College of Ophthalmologists workforce census 2018, flagged that there were 166 consultant posts currently unfilled (14% of all consultant posts) and that 17% of speciality doctor posts were also unfilled.3
The effect on preventable sight loss
It is estimated that around 22 people every month end up with severe or permanent sight loss due to delays caused by the capacity challenges the NHS currently faces.4 If demand grows as predicted, without significant investment or new ways of working, this number will continue to grow.
The role of diagnostic centres
NHS England has a stated aim to create diagnostic centres to improve access for patients to specialist care. In our view this is a misstep for two reasons.
Firstly, the capital investment needed to furnish these hubs with specialist ophthalmology diagnostic equipment and the specialist staff to staff them could be better spent on other parts of the NHS infrastructure.
Secondly, diagnostic centres do not address the challenge that elderly patients face in accessing care. Eye disease is more common in elderly patients and by virtue of the conditions, often prohibits patients from attending unaided to specialist services as patients often cannot drive to appointments because of their condition, or because of the treatment or investigations required. Diagnostic centres present the same barrier to access as hospital sites, in that they require family, friends, or carers to take patients. The NHS in some instances provides patient transport, but many patients report these as not fit for purpose as they cannot be accompanied by a carer, and the systems themselves are inflexible with early pickups and a late return home. The absence of appropriate support mechanisms requires the use of taxis or public transport, which may present a cost barrier or an accessibility barrier for those with eye disease. This is not a new or pandemic related problem as in a 2017 report by Age UK5 24% of those surveyed stated there was no form of appropriate public transport that could get them, or their loved one to hospital appointments on time.
In contrast optometric practices are located within the local communities meaning that if transport is required it is less costly, more familiar, and usually involves only a short journey of a few minutes. While diagnostic centres may make perfect sense for large multimillion pound pieces of equipment such as MRI scanners, optometric practices should be the location of choice for the majority of eye conditions, whether for treatment, management or diagnostic tests to inform management by ophthalmology.
How can optometrists help
Make better use of the optometric workforce
Optometrists are highly trained and regulated clinical professionals who work in well equipped, accessible practices. More importantly, by fully utilising the optometric workforce, the patient backlog could be tackled.
A national strategy for eye care is essential to making sure the clinical skills in optometry are used in full. It also ensures the following vital changes are made so more patients receive high-quality care, closer to home.
Empower optometrists to reduce avoidable referrals from optometric practice
Many referrals from optometric practice into secondary care are made because there isn’t a mechanism to perform repeat measures or referral refinement within optometric practice. This isn’t a limitation of skill or capacity, but instead a limitation of NHS commissioning.
By funding and commissioning enhanced services in the form of repeat readings in optometric practice, those patients who do not need referral can be kept out of secondary care reducing the inflow of new patients.
Provide a universal first point of contact in optometric practice
Universally commissioned NHS Minor Eye Conditions Services (MECS) or Community Urgent Eyecare Services (CUES) would allow optometrists to examine and treat a greater range of patient presentations without the need to refer to secondary care. By managing more patients at first point of contact and in a more appropriate, optometric setting, the flow of new patients into hospital services could be reduced.
Previous estimates suggest that ophthalmology outpatient first attendances could be reduced by around 500,000 (25%) and A&E, including eye casualty attendances for eye related problems could be reduced by around 350,000 (50%).
Move patients out of secondary care into optometric practice
Of the 7.5m ophthalmology outpatient appointments6, a significant proportion of these appointments could be delivered in optometric practice via one of three mechanisms.
- Autonomous management of patients using core optometric skills. Many patient presentations are suitable for management within optometric practice using core optometric skills Based on pre-pandemic research, it is estimated that 75% of patients who would otherwise have presented to their GP or to an eye casualty department can be successfully managed in optometric practice.7
- Autonomous management of patients utilising optometrists with higher qualifications. Optometrists with higher qualifications such as independent prescribing or specialist qualifications in glaucoma and medical retina, further increase the range of eye conditions that can be managed in optometric practice
- Semi-autonomous management of patients utilising synchronous and asynchronous connectivity. By utilising a detailed management plan produced by a specialist practitioner, which sets clear steps, goals, and criteria to work to, optometrists can semi autonomously manage 95% of patients. This provides a far wider workforce than currently exists within secondary care and would provide the biggest step to tackling the backlog
It is estimated that by simply moving low risk glaucoma patients into optometric practice that this could release around 200,000 appointments. However by utilising semi-autonomous management, more complex cases could also be moved into optometric practice potentially releasing double the capacity.
Ensure connectivity is an enabler and not a barrier
To deliver truly transformative new ways of working, it is essential that there is a genuine interconnectivity between optometry and the rest of the NHS. The current patchwork quilt of technology is inefficient, introduces risk and hinders collaboration. It is time to dispense with pilots and proof of concept and ensure that optometry and secondary care are truly connected.
Connectivity is the enabler for semi-autonomous management of patients whether this is via synchronous (real time) interaction with secondary care where the condition is time sensitive, or via an asynchronous interaction where a short delay is acceptable. For example, synchronous interactions would be necessary for patients with rapidly progressing, time sensitive conditions, such as wet AMD, but for generally slowly progressing conditions such as glaucoma, asynchronous interactions would still provide a safe patient outcome.
The latest hospital outpatient episode statistics suggest that around 1.75m patients underwent eye related imaging within a hospital setting.8 In the majority of cases those images could be captured within optometric practice, releasing secondary care capacity and tackling the challenge faced by patients in attending secondary care appointments.
References
- www.aop.org.uk/our-voice/policy/position-statements/2023/03/21/tackling-the-hospital-outpatient-backlog-in-eye-care
- www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/
- https://edgehealth.shinyapps.io/Ophthalmology_DF/
- www.rcophth.ac.uk/wp-content/uploads/2020/05/RCOphth-Workforce-Census-2018.pdf
- www.hsib.org.uk/news-and-events/latest-hsib-report-highlights-devastating-impact-of-delays-and-pressure-on-national-glaucoma-services/
- www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/active-communities/rb_dec17_painful_journeys_indepth_report.pdf
- www.aop.org.uk/our-voice/policy/position-statements/2023/03/21/tackling-the-hospital-outpatient-backlog-in-eye-care
- www.bmjopen.bmj.com/content/6/8/e011832
- www.digital.nhs.uk/data-and-information/publications/statistical/hospital-outpatient-activity/2020-21

