Our response to the Welsh Government proposals for reforms to eye care services
Our response to Welsh Government proposals for reforms to eye care services, June 2023
The AOP has submitted our response to the Welsh Government consultation on the reform of primary care ophthalmic services. Throughout our response we have considered the risks and benefits to patients and the profession. There is much to welcome in the reforms proposed by Welsh Government and we believe on the whole these will reduce waiting times, prevent avoidable sight loss and deliver better overall health and wellbeing for citizens of Wales. However, we think it is important to highlight where there are challenges and where further improvements could still be made.
Our response has been developed through a process of member and sector engagement including:
- A member survey (insight from which we have included in our response)
- Workshops (an in-person engagement session held in Swansea, and a virtual event for Welsh members who had been unable to attend the face-to-face session)
- Committees (AOP Policy Committee and Forums)
- Sector body meetings (regular sessions to explore common principles and socialise thinking)
- Social media (a range of interactive social media activity including Instagram, Facebook, and LinkedIn posts)
- AOP website articles
- Content in Optometry Today
- Press releases from the AOP
As we are a membership organisation, it is not surprising that member engagement formed a key part of our work in preparing to respond to the consultation. As part of this research we conducted a member survey. The survey yielded over 152 responses from optometrists from Wales who will be directly impacted by the proposed changes in Wales. Based on the figures published by HEIW, this represents approximately one in five optometrists in Wales.
In our response we have included qualitative and quantitative data from this survey and from the two member engagement sessions. Respondents to our survey provide a range of services to patients as shown in the table below:
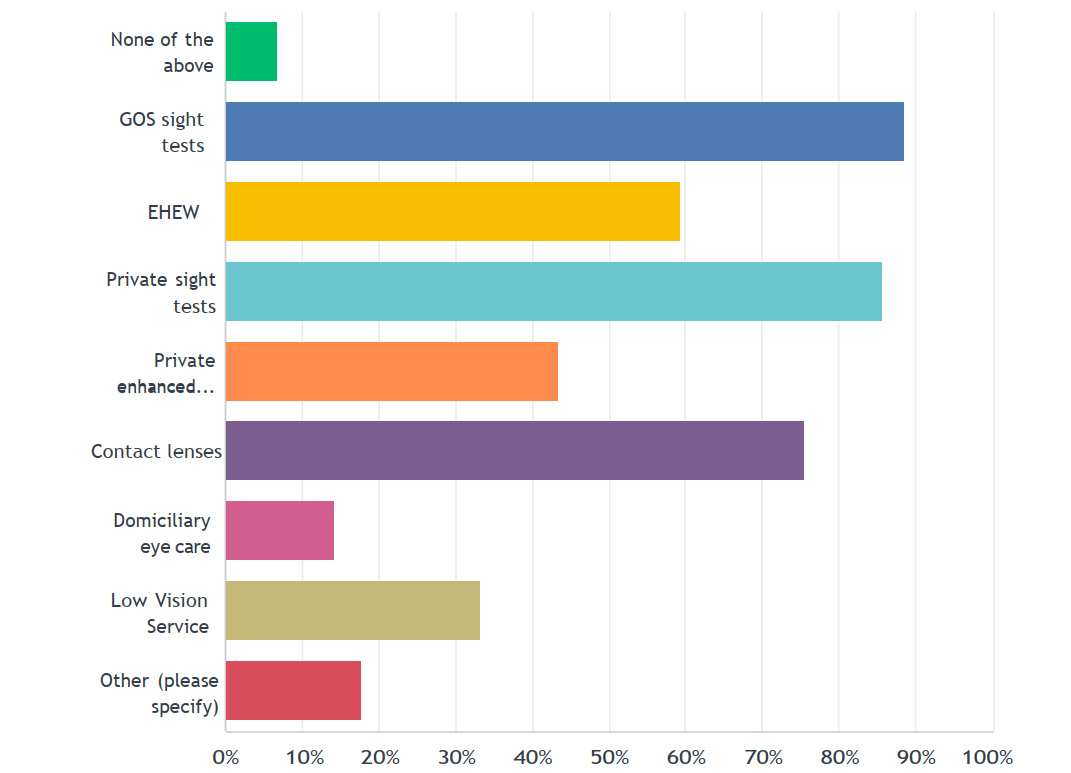
GOS sight tests – 88%, EHEW – 59%, Private sight tests – 86%, Private enhanced services – 44%, Contact lenses – 76%, Domiciliary eye care – 14%, Low Vision Service – 33%, and other services – 18%
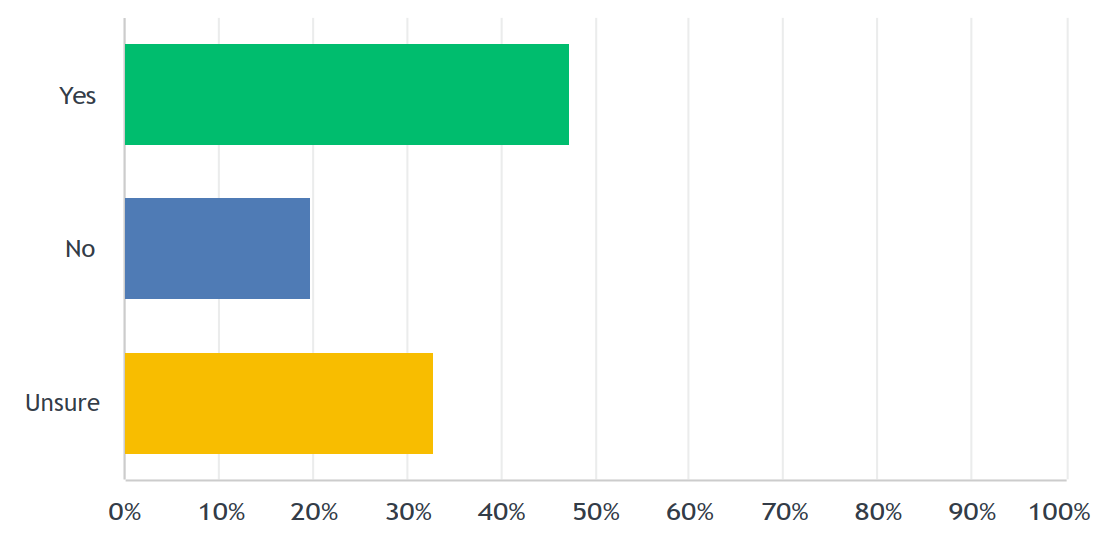
When asked if, overall, the proposals would improve access to eye care in Wales and improve patient outcomes, our members responded as follows:
43% of respondents said ‘yes’, 20% answered ‘no’, and a significant number, 37% said only ‘partially’
What members told us
Our response
Q1) Do you agree that optometric practices should be required to incorporate prevention and well-being advice as well as an individual patient management plan and patient self-care advice as part of the service they provide when providing an NHS sight test?
Yes. In broad terms, we are supportive given the general focus of clinical care in supporting wider health prevention and mental and physical wellbeing. Optometrists already have an important role in diagnosing conditions that are associated with lifestyle and health inequalities such as diabetes and hypertension. Being able to provide health advice and referrals such as smoking cessation and obesity is an important part of ill-health avoidance and ‘making every contact count’ (MECC).
It aligns with the ambitions set out in ‘A Healthier Wales’ published in 2018 and the ‘Future Approach for Optometry Services’ document published in 2021.
However, to fully implement these important areas, additional elements will be required to be added to the sight test performed in Wales. We broadly agree with the paper from the Welsh Government Optometry Contract Reform Group on this issue; however there are some uncertainties and therefore concerns about what this might look like in practice/operational terms and how far-reaching the scope for optometrists would be. For example:
- What could be undertaken safely and accurately within the current scope of the standard sight test time and as part of normal optometric practice? We suggest this is defined in future regulation and guidance
- How would any such health ‘screening’ interventions be deployed via ‘paper based’ health questionnaires such as alcohol and smoking cessation assessments? From available documentation, it appears that imaging technology for diagnostic assessment is out of scope of WGOS1. If it was added to be in scope, then it would need to be appropriately funded to cover all associated costs including maintenance
- The intention to include depression screening into the assessment role of the optometrists needs further exploration as to how optometrists will be trained in mental health assessment
Member opinion
“How long will NHS sight test need if prevention and health and well being advice included. What is "the development of an individual management plan" How onerous will paperwork/form filling be? There is already excessive amounts e.g. cataract referral 2 forms plus questionnaire plus copy of repeat prescription! Will need ways to make time more efficient e.g. less paperwork and better lines of communication with HES e.g. trying to do an emergency referral, phones currently often not answered so keep trying or send e mail but don't know if being actioned.”
The original intention of the contract reform process in Wales was to address the historic underfunding of the sight test. This was based upon the existing sight test service. Adding significant additional requirements to the standard NHS sight test would in our opinion require a far higher fee than is being suggested.
Q2) Do you agree that all optometric practices in Wales should offer an eye health examination to patients needing urgent attention or those at higher risk of eye disease?
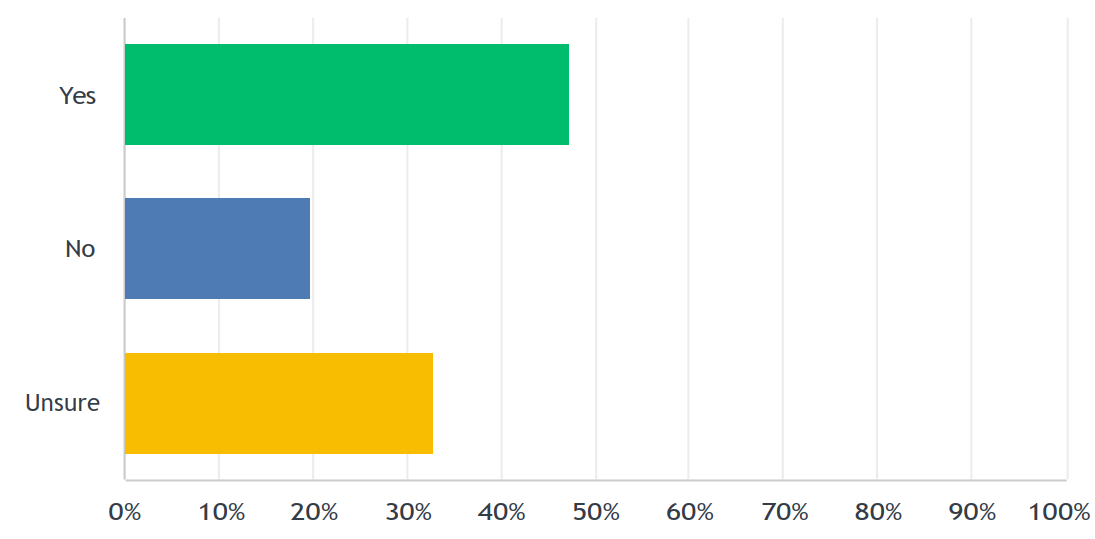
Yes. We believe that this will have a direct positive impact on capacity and demand in secondary care and in the early identification of eye disease. In our survey we asked members if they thought the proposals will reduce pressure on secondary care and reduce demand on GPs. As can be seen in the table below, 47% of respondents answered ’yes’, 20% said ‘no’ and 33% were ‘unsure’.
The principle is therefore broadly uncontentious and has received member support. However, we are concerned about the impact of these changes on the wider optometric market and the risks of eroding the provision of services in certain geographical areas. There is currently little clarity about how it is expected that smaller practices will meet a mandatory requirement. The requirement could have a differential impact on small or part-time practices – and some members have told us that it may lead to areas where there is reduced provision of service, choice and in some cases an absence of practices providing NHS examinations.
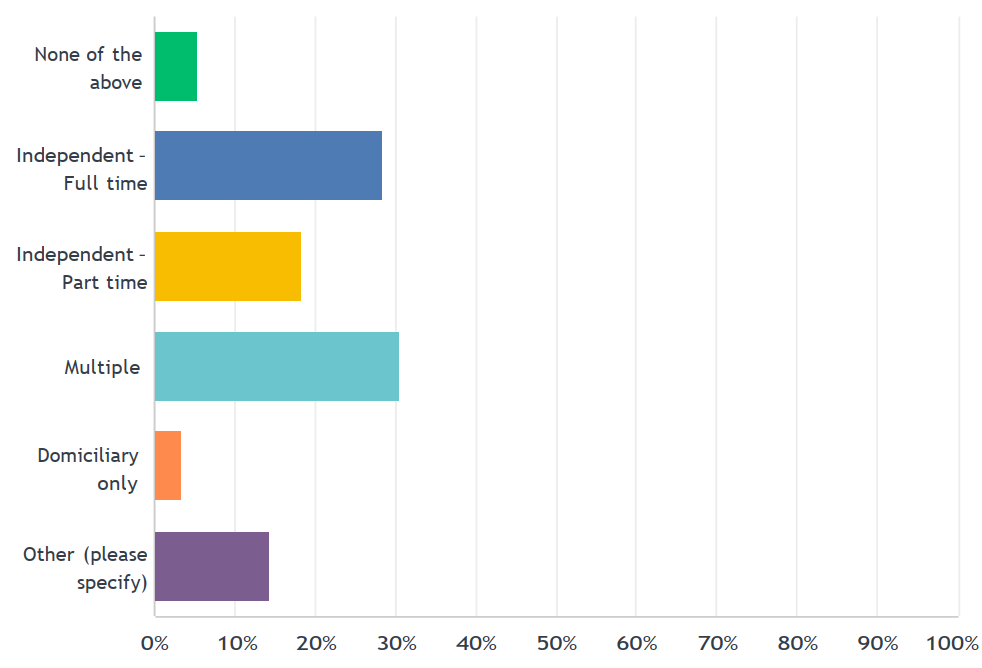
We received responses from optometrists working in a range of practice settings: Independent (full time) – 28%, Independent (part time) – 18%, Multiple – 30%, Domiciliary only – 3%, and other – 14%. Respondents also deliver a range of eye care services within their practice settings (see table 1 below). If we exclude those who aren’t in one of the more commonly defined groups, over 21% of respondents describe their practice as part-time. If these practices were excluded or forced to abandon GOS as a consequence of these reforms, there could be a significant impact on capacity.
Q3) Do you agree that all practicing practitioners in Wales must have a core standard of accreditation and training to enable them to provide the full range of core services including eye examinations?
Yes. Currently there is a strong provision of the optometric workforce across the country with the number of full-time equivalent optometrists being well-placed to take on additional roles. However, we agree with Optometry Wales that future need and the capacity of the eyecare workforce to meet that need is not currently understood. There is more work to be done to map current workforce data against population eye health data fully to understand the current and future need for core and enhanced community eye care provision. It should be noted that optometrists already have an approved and regulated core skill set. Building upon these skills is admirable, but this should only occur where there is genuine necessity.
Additional qualifications have the potential to add a significant cost burden as well as restricting access for the mobile, locum workforce on the border with England to provide services in Wales. This could have the unintended consequence of reducing the optometric workforce available in Wales. Given the proposals as set out in question two, if optometrists are increasingly to take on enhanced or extended roles as part of normal optometric practice, some modelling and assurances need to be demonstrated to ensure there is a sufficient workforce to deliver all elements of patient eye care.
Member opinion
“I feel too much pressure is being put on practice based optometrists. There are shortages of optometrists in Wales already, I know of optometrists near retirement age who are finishing early as the pressure is getting too much which will only increase the shortages. How will this serve the public when those years of experience are lost?”
“I can see it is good opportunity to advance clinical skills and the profession but currently not enough workforce.”
Q4) Do you agree with the requirement to have these proposed nationally directed services in primary care to ensure consistent access to eye care services across Wales?
The AOP has long advocated that a large proportion of the care that is currently delivered in a secondary care setting could, and indeed should, be delivered in primary care. As such we are supportive of these changes. However, we have some concerns about how it will be determined who should be able to provide the higher levels of care and advocate that this should be open to all who have the necessary skills and equipment.
Q5) Do you agree that a practice who doesn’t offer higher-level clinical services should be legally compelled to refer a patient to a nearby practice who does offer the necessary clinical services to meet the needs of the patient?
Yes in principle, we support a model of standard and enhanced community eye care. However, this in principle support needs to be tempered by a clear element of caution. We feel further clarity of explanation is required.
Based upon our survey AOP members were broadly supportive of this approach with 69% saying they ‘agree’ and 32% saying they ‘disagree’.
We are nervous about practices being subject to legal compulsion in this area, as success will be dependent on a number of external factors such as the geographical location and proximity of some practices to each other, boundaries of local health board (LHB) areas, the availability of suitably trained staff on the day, and patients’ ability and willingness to travel.
This change will also require additional protections to ensure that where a patient is redirected for one aspect of care, they are signposted back to their normal practice for other aspects of care. This protection will ensure continuity of care is provided and reduce the risk to patients.
Q6) Do you agree that a duty should be placed on optometry practices to collaborate to ensure the eye health needs of the cluster area are addressed within primary care clusters?
In principle, we support such a duty. However, while the revised fee structure provides extra remuneration for the majority of clinical practices, it is not clear that the proposed fee level is sufficient to enable true collaborative working, as doing so imposes additional unfunded reporting burdens. Therefore, while we are supportive of the aim and direction, further detailed work has to be done to manage the risk that business logistics for practices may ultimately hinder implementation.
More generally, effective integration is a key element of the future delivery of community-led primary care. However there is often disparity of representation of primary care professions and members report that representation and associated funding of optometry at ‘cluster’ level is currently inconsistent. Given how important cluster working will be in future, these need to be remedied. We agree with the wider narrative of these reforms which suggest a health board-wide approach to cluster activity is preferable.
We feel that the adoption of the recommended cluster model more widely suggested during discussions, may help address some of our members’ concerns about consistency of access, especially for the most vulnerable patient groups.
Q7) Do you agree it would be beneficial for LHBs to conduct an eye health needs assessment every three years to ascertain the specific needs of their communities, with a duty imposed on LHBs to do so to bolster this provision?
We agree there is a benefit to LHBs undertaking an eye health needs assessment. We feel every three years is excessive, as it could cause additional amounts of work that isn’t required. Anecdotally we heard this was the case in pharmacy when a three-year assessment period was imposed.
Ultimately, we feel a period of five years would be better. However, given the scale and planned associated impact of these reforms, we would suggest a ‘rapid review’ be undertaken across all change themes after one year, and the results published and socialised with the sector, with a view to additional amendments or ‘tweaks’ to policy and clinical delivery to resolve any issues identified, and implement any necessary measures to deliver the best possible patient outcomes. It also goes without saying that any review period agreed following implementation doesn’t remove the need to address the issues members have raised as needing to be addressed prior to implementation.
Q8) Do you agree with the introduction of one Ophthalmic List per LHB to reduce complexity?
Yes, the proposal to have a single list of contractors and performers is sensible. However, we suggest that a national list with a marker to indicate the LHB in which practitioners work may be more useful from a planning perspective. Broadly this becomes a discussion about whether you collate a list from local information, or gather once, nationally, and disseminate. We would favour the latter as in our opinion it provides a more uniform user experience and reduces the risk of duplication.
Q9) Do you agree with the proposal for LHBs to produce an additional administrative amalgamated list of all individual practitioners who are registered on their ophthalmic list and perform NHS ophthalmic services?
Yes, but we reference our point above at question 8 about how this may be approached.
Q10) Do you agree with the proposal to include student optometrists registered with the GOC, within the supplementary ophthalmic list, to ensure appropriate oversight and governance arrangements are in place?
We disagree with this proposal. The GOC is considering removing the requirement to register students and it is expected that wider reform by DHSC is likely to remove this requirement from healthcare regulators. To introduce a requirement that is contrary to this direction of travel seems counter intuitive.
Q11) Do you agree with the proposal for LHBs to produce an administrative list of all dispensing opticians who provide NHS services in their area?
Yes, but as for optometrists, it is our opinion that the list should be collated nationally and disseminated, rather than collected regionally and amalgamated nationally.
Q12) Do you agree that all NHS funded contractors / opticians, should offer core clinical hours as agreed between the contractor and their LHB to ensure suitable access to patients?
It is unclear what this question means. If there is a requirement for national minimum core hours, that could force small providers and part-time practices to cease providing NHS services due to unviability. However if the intention is that these core hours will be flexibly negotiated on a case-by-case basis in conjunction with contractors, then we are supportive.
Our member survey reflected a similar lack of clarity with regard to access to eye care services; 33% within this cohort of practices thought ‘access would increase’, 28% thought ‘access would partially increase’, with 17% thinking it would ‘not increase access’ and 22% ‘unsure’.
We note that the paper on rurality has not been published and it would seem that understanding this need is an essential part of any service provision requirements.
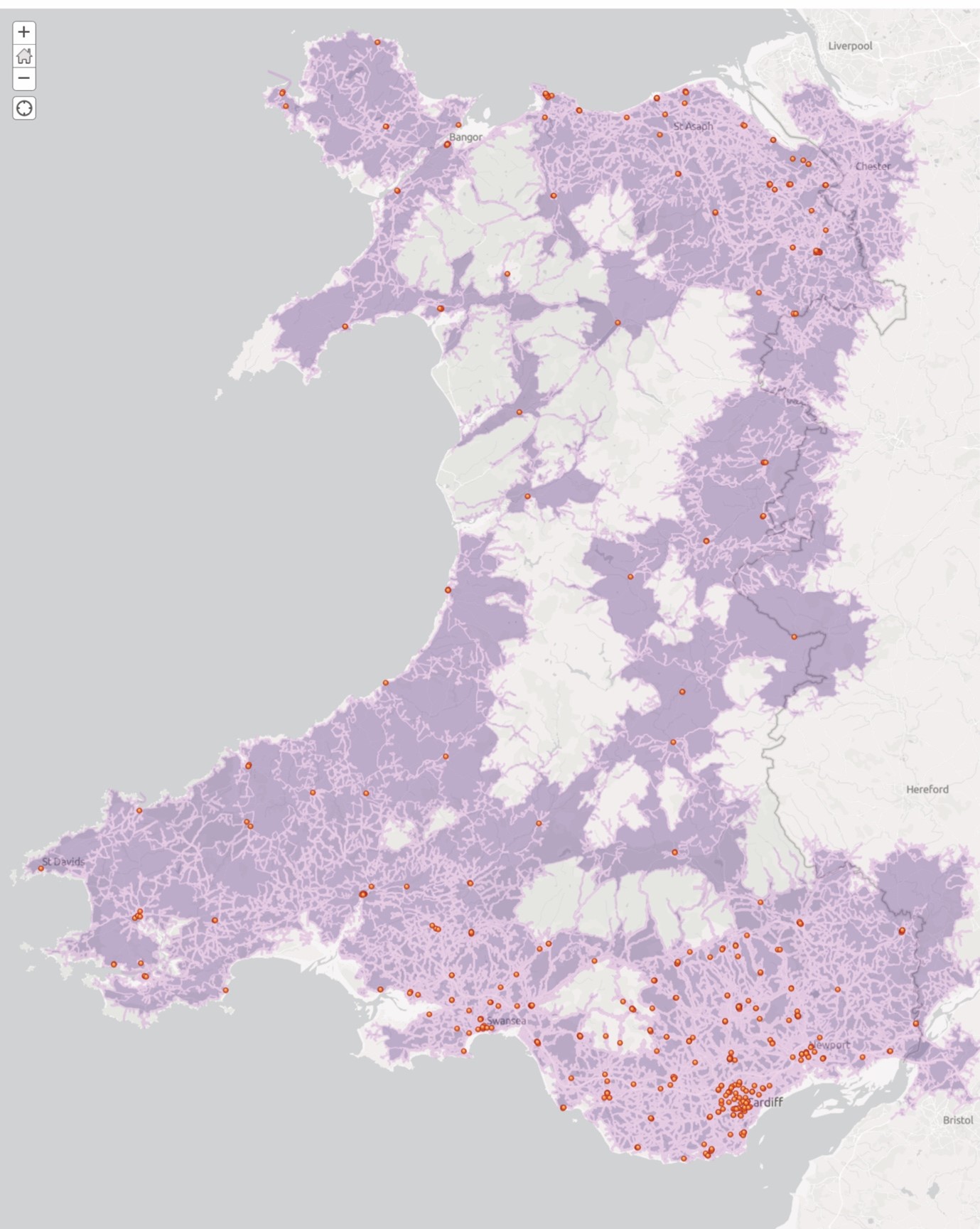
Figure 1 AOP produced map of practice location and calculated driving times using mapping software
When the practice locations within Wales are plotted (red dots), it is clear that in many areas there are only one or two practices providing services to large sparsely populated areas. If any of these are forced to cease GOS provision, it is likely that significant areas will be left without NHS eye services. Further, if we look at the area within 20 minutes’ drive from practice locations (purple shading), we can see that the coastal areas and central belt are under significant risk should practices close or leave GOS. Even in areas that are less densely populated, it is essential that these patients still have sufficient service provision as these areas often contain rural poor, isolated and vulnerable individuals.
AOP survey data shows that for part-time independent practices, 22% thought the reforms would negatively impact their practice finances and 50% did not answer positively or negatively, indicating a significant level of uncertainty.
Member opinion
“I work part time and have an understanding employer that lets me switch dates to suit family and other commitments…….Rural practices especially part time practices really not given much consideration. We provide a valuable service to rural communities but risk that practices may close or have to amalgamate 2-3 part time to create one full time practices making px travel further for services.”
Q13) Do you agree with our proposal to remove the advance notice requirements that contractors must provide to Local Health Boards prior to undertaking mobile services?
Yes. We believe the advance notice requirements create inequity for patients and serve no purpose. Removing them will improve patient access to care and allow for more timely interventions. In our member survey 87% of respondents said they ‘agreed’ with the proposal to remove the advance notice requirement.
Q14) Do you agree with our proposal to expand further the provision of mobile eye care services to qualifying patients who are unable to receive care in an optometry practice?
Yes, but we point out that there are logistical challenges within a domiciliary setting that must be considered. It is essential that requirements with regard to time periods and equipment levels are sensitive to these logistical challenges. Overly onerous criteria could actually reduce the level of service provision rather than increase it. Further, the level 2 WGOS fee alone is unlikely to meet the cost of care provision, especially if the same time periods are expected as in fixed practice locations.
There was real doubt among our members, especially those who provide domiciliary and low vision services, about the potential impact of these proposals. In our survey, when our members were asked to think about domiciliary patients, and how these proposals would affect the accessibility of the services they need, only 13% said they felt it would ‘deliver a better service’, 26% thought it would be ‘worse’, 20% thought it would ‘be the same’ with a further 38% ‘unsure’ about the impact on their patients. In our survey, 87% of respondents said they would be in favour of expanding mobile eye care services for those unable to receive care in optometric practice, with 14% saying no. 84 people were unable to answer yes or no to this question, suggesting significant uncertainty regarding the impact these changes will have on their patients. We cover the issue of domiciliary eye care services in question 21 below.
Member opinion
“Although the proposals may have some benefits in a practice setting, as a domiciliary provider only and part of the Low Vision Service, all aspects of our NHS services have been affected in a negative way. My concern is not only will domiciliary providers stop providing the service, practices who perform domiciliary eye examination will also stop and ultimately vulnerable housebound patients will suffer”.
Q15) Do you agree with the additional safeguarding measures proposed? We would welcome your views as to whether practitioners should register with and maintain annually the DBS Update Service or alternatively for practitioners to have a new DBS certificate every three years?
It is our opinion that there is already UK-wide legislation that sets out when a DBS check is required, and safeguarding requirements should reflect this wider legislation. The proposed change broadly aligns with our understanding of this wider legislation and as such we are supportive. On the specific question about the DBS update service, the AOP suggest that practitioners undertaking DBS checks sign up to the DBS update service as this ensures a current DBS certificate is available whenever it may be required. Examples of this requirement would include when changes of employment occur.
There is a further consideration in this regard in that there may be a significant volume of practitioners that require DBS checks. This process could take some time to complete and we advocate for a sensible transition period to avoid introducing an unnecessary burden for practices.
Q16) Do you agree with the proposal to impose a requirement on NHS contractors / opticians to use electronic referral methods where available to ensure timely access to eye care services?
The use of electronic referral is uncontentious in principle and has been a longstanding request on behalf of the wider optical sector. It brings well-documented potential benefits regarding improved data gathering, education and service planning.
There are however challenges associated with implementing electronic referral that must be addressed. These include but are not limited to:
- The need to ensure maturity of systems across the whole estate. It is not enough to simply mandate electronic referral if the other parts of the system are not ready to receive data and feedback via this mechanism
- The need for robust failsafe procedures in the case of system outage
- The need for sufficient training and support to aide all practitioners in the use of new systems
- There was wide agreement that these changes must not add an additional time burden to care delivery. This includes as far as is possible a reduction in double keying via the use of APIs and the streamlining of all processes. The fees suggested as part of the reforms reflect a like-for-like service with regard to sight testing. If electronic referral increases the time required, it would be necessary to reflect this additional time in the proposed fee
Member opinion
“These changes should only come into place with an active computerised referral system for North Wales, which has yet to materialise 3 years on from the proposed, virtually guaranteed date they gave. I don’t much like how we don’t have a choice either.
Q17) Do you agree with the above proposals to improve governance and quality standards for Optometry in Wales? Please elaborate if you think this is reasonable and proportionate. You are welcome to comment on each item in isolation (from a-d) or provide a general response across the range of proposals.
It is unclear why Quality for Optometry (QO) will become a yearly requirement and it is further unclear if this additional administrative burden has been reflected in the proposed fee structure, as it appears separate to the documented governance changes.
Further, it is also unclear why despite Quality in Optometry (QiO) existing as a sector wide, agreed, developed and proven governance requirement, the consultation appears to suggest for that there isn’t any form of existing governance for optometric practices. With regard to each contractual aim, we have the following comments:
a) Feels overly burdensome and disproportionate to the risk
b) Is admirable, but could be a significant undertaking for large practices with large staff numbers
c) Is reasonable as long as an efficient mechanism for reporting and updating is created. This process should not be burdensome. If it is and the data lacks currency, then this will undermine the aspiration
d) Is unclear, it is presumed that it is three audits across both domains, not three for each domain, but as the scope, scale and content of these are undefined it is not possible to agree to this requirement at this point. Once full detail is provided, we would be happy to consider whether these proposals are appropriate
Q18) Do you agree that eligible patients should be entitled to a free optical appliance across all prescription ranges with a duty placed on contractors to support this free provision?
It is an admirable concept that all patients of limited means should be able to obtain optical appliances without necessarily having to contribute towards them. As such we are supportive of the principle. But we have very serious concerns about the implementation. The proposal to reduce voucher values cuts across the principle and undermines its effectiveness. These cuts, in conjunction with a level of inflation unprecedented in recent times, mean that many practices will struggle to meet this requirement at all. Others will only be able to provide such limited choice as to be broadly meaningless.
The AOP member survey, together with feedback from our member engagement events, showed that a strong majority of members predict that the changes to voucher values will have negative consequences for the poorest of their patients. Approximately 64% of members stated they would need to decrease the range of spectacles they offered on a voucher due to the proposed changes, leading to a reduction in patient choice for the poorest.
When asked which patients would be better served by these proposals and which would not, the results were as follows:
- From an accessibility perspective 29% of those who responded thought access to services would increase for patients with glaucoma, mainly driven by the positive view of the aim to deliver more glaucoma care in a primary care setting
- For patients who receive a GOS 3, over 40% of respondents thought access would decrease, and this reflects the concerns around the reduced voucher values
- This result was broadly replicated when we asked members about choice; over 40% of members had concerns about the impact on patient choice of appliance if voucher values are reduced
- When we asked members about how they thought the proposals would impact upon cost, around 65% of respondents thought patients who receive a GOS 3 would be worse off
Member opinion
“The border funding needs to be sorted. I cannot claim a WECS because I do not practice in Wales, and I cannot claim a CUES for patients with a Welsh GP. If I weren’t socially and ethically responsible, the HES would be seeing a LOT more patients. I usually average 3 ‘emergencies’ a day, personally, though not all cross-border”.
“The reduction in voucher values will result in less patient choice and a reduction in quality of spectacles because the values do not cover the frame/lenses/glazing/postage & dispensing fees”.
When we consider the impact on different patient groups these challenges become clear. For example, for a practice who mainly sees patients who are eligible for an NHS-funded sight test, but pay privately for their spectacles, these changes will see a significant increase in the level of remuneration the practice receives, as the sight test fee will rise from £21.71 to £43.00 or a 98% increase in the fee received. As this example patient pays privately for their spectacles there is no change in that regard.
However, for a practice that mainly sees patients who are eligible for NHS sight tests by virtue of being on means tested benefits, the situation is quite different. This is especially true for practices with an older patient base, who require both distance and near spectacles.
For example, currently a practice seeing an older patient for a sight test and providing distance and near spectacles, receives £21.71 for a sight test and £39.10 for each pair of spectacles giving a total NHS funded remuneration of £99.91. In contrast under the proposed reforms, the sight test and vouchers would provide only £87, which is a decrease of 13%. This is before any consideration is given to the additional reporting requirements, which are also part of the reforms.
This creates a risk that the most vulnerable in our society, those of limited means and in some cases the most in need of optical appliances, will be deprived of a choice of appliance, choice of practice, or provided with an appliance that is not robust enough to fulfil their needs until they are eligible for a replacement.
Member opinion
“Whilst I welcome the changes to sight test and enhanced services fees, I am disappointed in the proposals of the decrease in spectacle vouchers. The ones which will suffer the most are people on means tested benefits and families with children. Practices will be forced to reduce their ranges of frames which can be provided free of charge with the voucher. This may lead to children not wearing their spectacles as are unhappy with choice. It could lead to patients on benefits suffering with anxiety and depression and will not give them as much option to upgrade to lenses such as high index, sunspecs etc within their budget. It may lead to patients preferring older specs and not updating their prescriptions as regular which would impact their vision and quality of life. Practices will maintain their prices and the patients will be the ones to suffer the impact of the extra cost which I think is very unfair especially in the current climate with the cost of living as high as it is”.
“The reduction in voucher values will result in less patient choice and a reduction in quality of spectacles because the values do not cover the frame/lenses/glazing/postage & dispensing fees.”
This situation is even more concerning within the domiciliary setting. Domiciliary care obviously involves travelling to the patient’s home. Given the geography of Wales, in some instances that travel may take a significant amount of time. For good quality care, optical appliances should be delivered and fitted, to ensure patients are aware of how to use and care for them. This means the significant periods of travel are not simply an issue when conducting a sight test, but also when delivering the appliance.
While there is a proposal to raise the sight test fee to address historic underfunding, there is a proposal to reduce the domiciliary fee for many. The proposed reduction to the voucher values further increases pressure. Taking our same example above of a patient eligible for an NHS sight test and NHS vouchers towards spectacles, and adding the changes to the domiciliary visiting fee, for first and second patients, those more likely to be seen within their own homes provides the following example:
- Current situation £99.91 + £38.27 = £138.18
- Proposed reforms £87 + £26 = £113
This represents a staggering 18% reduction in the total NHS remuneration for this critical patient service.
Children are another patient category that are likely to be affected by the change to vouchers. A decreased range of spectacles risks stigmatising spectacle wear in a way not seen since the abolition of “NHS glasses” in the 1980s. This potentially retrograde step could hinder education and risk eye problems such as amblyopia going undetected. The need to contribute to spectacles in a way that is largely unnecessary at the current voucher level, means an additional cost burden for already stretched family budgets. Closely linked to this issue is the topic of spectacle repairs. Children are recognised as being hard on their spectacles, and many break them regularly. If an additional fee is required each time the spectacles are broken the cumulative effect of this additional burden may be prohibitive even for those who on a single instance can and do choose to “top up”. In a common scenario where a child breaks their spectacles five times per year and has to “top up” each time it is feasible that this amounts to a hidden patient tax of £100 per year.
Having reviewed the published documents for this consultation there does not appear to be a proposal for the new spectacle repair costs. If we presume they will reflect the apportionment seen in the existing repair provision, a replacement side will be paid at £4.14. This is likely to be less than the cost of a replacement frame. But budget frames are not normally available as parts. This means a whole frame must be ordered. Once postage is included and ignoring overheads, these costs alone will mean that the voucher does not cover costs to the practice of the repair or replacement. This is likely to add another burden to parents. A similar scenario exists for all part replacements such as a single lens.
It is also likely that the need to order a whole frame rather than parts will lead to increased costs to the NHS and a larger amount of “plastic” materials heading to landfill.
In summary, we have very serious concerns that the reduced voucher values in conjunction with a requirement to provide an appliance for that value, may reduce service, quality and in some areas lead to a reduction in capacity. Given the projections around an ageing population and the desire to ensure that as people age, they stay in their own home as long as is possible, we are concerned that these patients may not be able to obtain care. This could the widen health inequalities gap.
Member opinion
“It is not at all clear why families with children, people on means-tested benefits, and the most vulnerable are the only groups being targeted to pay for reform by reducing voucher values”.
“I am very concerned about domiciliary eye care services. Many providers [are] thinking about stopping services and how the new contract is going to work moving forward. Coming after covid when things have been especially challenging, Domiciliary eyecare is now trying to survive not thriving. In an ageing population, with more domiciliary demand, it almost seems as if domiciliary eyecare is being sacrificed to push through the new contract. There has to be a core of domi providers to be able to offer and maintain domi appointments and services. The new contract is going to make virtually impossible.”
“I am very concerned over the future of domiciliary services in Wales and ultimately concerned that some of our most vulnerable members of our society will suffer. We have a chance to make some positive changes to our profession but NOT at the cost of our domiciliary services and low vision services.”
Q19) Do you agree with the above proposal to extend the eligibility criteria to certain prisoners on leave?
Yes, but we reiterate our concerns around the proposed changes to vouchers as they are even more important with regard to this group, who are even less likely to have the means to top up their purchase to achieve a robust appliance.
Q20) Do you agree with the above proposal to extend the eligibility criteria for under 18-year-olds who are care leavers or are in the care of a Local Authority?
Welsh Government estimated that there were 700 young people aged 16 and over leaving care between 1 April 2021 and 31 March 2022, representing an increase of 24 young people (4%) compared with the previous year. This is a significant number of vulnerable young people who will need extra support.
We are therefore supportive of this proposal but we reiterate our concerns around the proposed changes to vouchers as they are even more important with regard to this group, who are less likely to have the means to top up their purchase to achieve a robust appliance.
Q21) We would welcome your thoughts as to whether you think there are any other benefits or disadvantages not mentioned in the consultation? Please explain what these might be and provide evidence to support your response.
Domiciliary fees as mentioned under Q18. The changes to the domiciliary fee create a significant challenge to care delivery. Domiciliary visits have historically been paid at two rates: a higher rate for the first and second patient at an address and then a lower rate for the third and subsequent patients at an address. This situation was intended to address the travel costs which are proportionally higher when travelling to an individual’s home to see one or two patients in comparison to travelling to a residential or care home where those costs are relatively lower, as multiple patients are seen without the need to set up and pack away the equipment multiple times.
By proposing a flat fee for domiciliary care, these proposals disincentivise the delivery of care within a patient’s own home, while making the delivery of care within a care home relatively more attractive. While those in a care home are likely to require a greater amount of care than those in their own homes, this is not a universal truth and even if it were, the support networks around patients within a care home are greater. That leaves those patients who are housebound at risk of reduced access to care, potentially longer waiting times to receive care and higher costs. We urge Welsh Government to reconsider these proposals and to consider the changes suggested in the letter recently sent by the Domiciliary Eyecare Committee (DEC).
Low vision service provision requires significantly greater clarity. It is not possible to tell from the published documents who will be eligible for which fee level. Wider presentations from Welsh Government suggest an additional low vision domiciliary fee will be available, but the qualifying criteria are not clearly set out. If follow-up visits do not attract a supplementary fee on top of the £53 suggested, many providers will no longer be able to offer this vital and already undervalued service. The AOP and our members would welcome clarity on this matter. If an additional visiting fee has been overlooked, we hope that Welsh Government will rectify this as a matter of urgency.
Q22) The Welsh Government is committed to creating an environment where everyone will want to use the Welsh language. We would like to know your views on the effect the new legislation could have on the Welsh language, specifically on opportunities for people to use Welsh and on treating the Welsh language no less favourably than English. What effects do you think there would be? How could positive effects be increased, or negative effects be mitigated?
No comment.
Q23) Please also explain how you believe the proposed legislation could be formulated or changed so as to have positive effects or increased positive effects on opportunities for people to use the Welsh language and on treating the Welsh language no less favourably than the English language, and no adverse effects on opportunities for people to use the Welsh language and on treating the Welsh language no less favourably than the English language.
No comment.
Q24) We have asked a number of specific questions.
Please find below other feedback from members in Wales received as part of our consultation survey.
How do you expect the proposals to affect the services you currently provide? Explanatory note – For example, will it be more difficult to provide the service or provide the service at the same level as you currently do?
| Considerably harder to provide | Somewhat harder to provide | About the same | Somewhat easier to provide | Considerably easier to provide | |
| GOS sight tests | 16.25% 13 |
16.25% |
46.25% 37 |
16.25% 13 |
5.00% 4 |
| EHEW | 14.86% 11 |
8.11% 6 |
56.76% 42 |
17.57% 13 |
2.70% 2 |
| Private sight tests | 6.58% 5 |
11.84% 9 |
80.26% 61 |
1.32% 1 |
0/00% 0 |
| Private enhanced services | 13.34% 9 |
10.29% 7 |
69.12% 47 |
7.35% 5 |
0.00% 0 |
| Contact lenses | 4.17% 3 |
5.56% 4 |
88.89% 64 |
1.39% 1 |
0.00% 0 |
| Domiciliary | 29.41% 15 |
7.84% 4 |
45.10% 23 |
15.69% 8 |
1.96% 1 |
| Low vision services | 19.12% 13 |
10.29% 7 |
57.35% 39 |
13.24% 9 |
0.00% 0 |
Will you need to make adjustments to your service provision as a result of these changes? For example:
| Considerably decrease | Somewhat decrease | About the same | Somewhat increase | Considerably increase | |
| Clinical sessions | 3.90% 3 |
14.29% 11 |
55.84% 43 |
22.08% 17 |
3.90% 3 |
| Staff employed | 2.74% 2 |
9.59% 7 |
63.01% 46 |
19.18% 14 |
5.48% 4 |
| Range of services | 6.67% 5 |
10.67% 8 |
36.00% 27 |
37.33% 28 |
9.33% 7 |
| Range of spectacles offered | 9.86% 7 |
14.08% 10 |
61.97% 44 |
11.27% 8 |
2.82% 2 |
| Range of spectacles offered for a voucher | 42.47% 31 |
21.92% 16 |
26.03% 19 |
8.22% 6 |
1.37% 1 |
| Price of spectacles | 5.48% 4 |
4.11% 3 |
50.68% 37 |
32.88% 24 |
6.85% 5 |
Thinking about the patients you serve, how will the proposals affect the CHOICE of the services they need?
| Better | Worse | Same | Unsure | |
| Patients with low vision | 16.88% 13 |
15.5% 12 |
49.35% 38 |
18.18% 14 |
| Children | 7.69% 6 |
23.08% 18 |
52.56% 41 |
16.67% 13 |
| Patients under 40 on low income (GOS3) | 5.19% 4 |
41.56% 32 |
37.66% 29 |
15.58% 12 |
| Patients over 40 and under 60 on low income (GOS3) | 5.19% 4 |
42.86% 33 |
36.36% 28 |
15.58% 12 |
| Patients over 60 eligible for GOS3 | 6.49% 5 |
38.96% 30 |
38.96% 30 |
15.58% 12 |
| Patients over 60 not eligible for GOS3 | 10.26% 8 |
7.69% 6 |
67.95% 53 |
14.10% 11 |
| People with glaucoma | 36.36% 28 |
3.90% 3 |
41.56% 32 |
18.18% 14 |
| Domiciliary patients | 16.92% 11 |
20.00% 13 |
29.23% 19 |
33.85% 22 |
| Patients with learning difficulties | 5.26% 4 |
9.21% 7 |
51.32% 39 |
34.21% 27 |
| Prisoners | 11.43% 8 |
4.29% 3 |
27.14% 19 |
57.14% 40 |
| Homeless people | 5.56% 4 |
5.56% 4 |
38.89% 28 |
50.00% 36 |
Thinking about the patients you serve, how will the proposals affect the COST of the services they need?
| Better | Worse | Same | Unsure | |
| Patients with low vision | 5.19% 4 |
18.18% 14 |
53.25% 41 |
23.38% 18 |
| Children | 3.85% 3 |
47.44% 37 |
34.62% 27 |
14.10% 11 |
| Patients under 40 on low income (GOS3) | 6.49% 5 |
61.04% 47 |
22.08% 17 |
10.39% 8 |
| Patients over 40 and under 60 on low income (GOS3) | 5.13% 4 |
65.38% 51 |
19.23% 15 |
10.26% 8 |
| Patients over 60 eligible for GOS3 | 6.41% 5 |
62.82% 49 |
20.51% 16 |
10.26% 8 |
| Patients over 60 not eligible for GOS3 | 7.69% 6 |
19.23% 15 |
61.54% 48 |
11.54% 9 |
| People with glaucoma | 11.54% 9 |
8.97% 7 |
61.54% 48 |
17.95% 14 |
| Domiciliary patients | 7.58% 5 |
22.73% 15 |
33.33% 22 |
36.36% 24 |
| Patients with learning difficulties | 6.49% 5 |
18.18% 14 |
41.56% 31 |
33.77% 26 |
| Prisoners | 11.43% 8 |
8.57% 6 |
27.14% 19 |
52.86% 37 |
| Homeless people | 7.04% 5 |
8.45% 6 |
36.62% 26 |
47.89% 34 |
Do you think overall the proposals will impact positively or negatively on your practice finances?
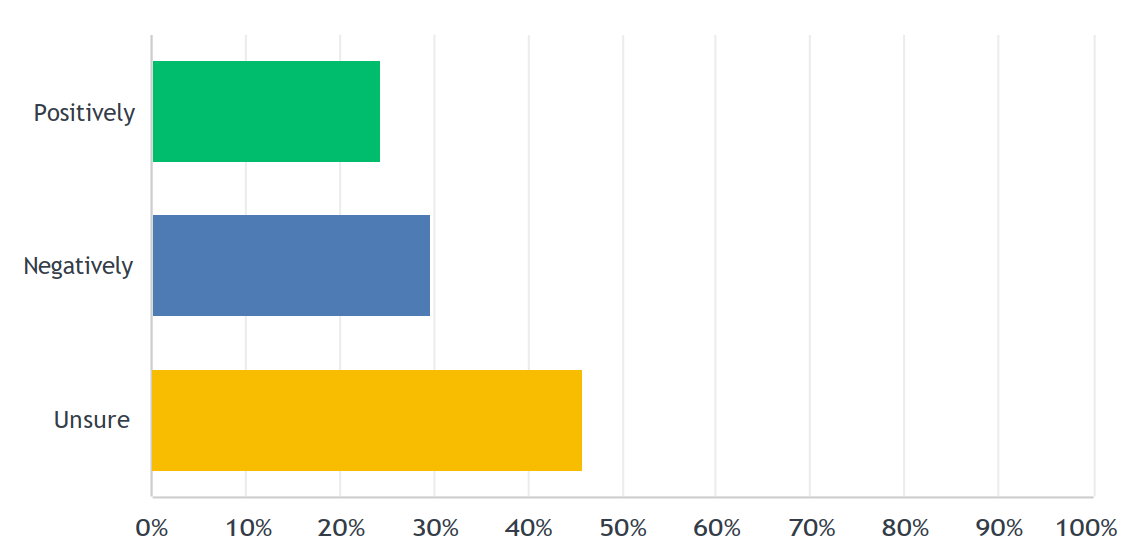
(Positively – 24%, Negatively – 30%, and Unsure – 46%)

