- OT
- Life in practice
- Practitioner stories
- “The seriousness of my situation began to dawn on me”
An optometrist saved my life
“The seriousness of my situation began to dawn on me”
Practice owner and optometrist, Dr Martin Smith, and a patient from his Lincoln practice discuss a referral for a retinal tear
7 min read

16 September 2021
Before you went for a sight test, had you experienced any symptoms and how had this affected you in day-to-day life?
Patient LB: I contacted Dr Smith as I had experienced a lot of floaters three weeks before, which had then subsided. I also experienced some flashes of light at the bottom of my right eye occasionally.None of these symptoms affected my day-to-day life and I wondered if I was wasting everyone’s time. But I felt I should get my eyes checked, so I contacted Dr Smith, who saw me the following day.
What did the optometrist find, and how did they explain the next steps to you?
LB: Dr Smith examined my eyes, using several different types of scans. He explained that he had found a tear across the retina at the top of my right eye and showed me a photo of it. He said it would need urgent treatment to repair it. He contacted the local hospital and told me I should go straight away to be assessed. He did not alarm me, but was insistent I should not delay. I went to the hospital the same afternoon.Can you describe how you felt during the referral?
LB: At the local hospital they were concerned and referred me to Queen’s Medical Centre (QMC), Nottingham University Hospitals, for urgent treatment. I was quite surprised at the extent of the problem, but glad that something was going to be done about it as soon as possible. The seriousness of my situation began to dawn on me and I did not want to think about the possibility of losing my sight, which was very frightening.Before this happened, blindness was something that happened to other people and I took my sight for granted. I now realise how quickly things can change and I will be more aware of this in future
Did you have to undergo further treatment and what has been the outcome?
LB: At QMC I underwent an operation under local anaesthetic. The vitreous jelly was sucked out of my eye and the tear was repaired using, I believe, a freezing process. A bubble of gas was then inserted into my eye to press the retina back into place. I had to keep my head facing down for 24 hours and then keep it erect, as the tear was at the top and the gas bubble would hold the retina in place. I also had to rest and insert eye drops four times a day.I returned for a check-up after two weeks, when all was well. I have since had a further check-up now that the gas bubble has dissipated and have a final check-up scheduled. To date, all is going to plan and my sight, which I lost after the surgery, has returned.
Have your views on the importance of sight tests and eye care changed as a result of this experience?
LB: This experience has definitely changed my views on the importance of eye tests and eye care. Before this happened, blindness was something that happened to other people and I took my sight for granted. I now realise how quickly things can change and I will be more aware of this in future.How has the experience changed your life or affected you?
LB: This experience has made me very thankful to all those who were able to save my eyesight and thankful for the advances in technology now available. I really don’t know how people cope with losing their sight, which to me would be one of the worst things that could happen, health-wise.We have seen a much wider range of clinical and emergency care during the pandemic and my independent prescribing qualification has been very useful
How has COVID-19 affected your practice? How did you adjust your services to be able to meet the needs of your patients?
Dr Martin Smith, practice owner and optometrist at Martin Smith Opticians (MS): Following the initial period where we were open only for essential and emergency care, we have been very busy. Longer appointments due to increased infection control have necessitated continuing prioritisation of care and patient triage. We are keeping appointments deliberately free until late notice for patients who need to be seen quickly, like in this case. We have seen a much wider range of clinical and emergency care during the pandemic and my independent prescribing qualification has been very useful. The introduction of our eye plan scheme encourages patients to use us as the first point of contact for eye problems.Have you introduced any technologies or systems that have helped your interactions with the patient and how you carried out the sight test during COVID-19?
MS: We immediately identified that a face-to-face consultation appointment was necessary from the triage. I am always very keen to see flashes and floaters as soon as possible as I have seen several tears with very few symptoms. In this case the initial symptoms had almost resolved but we triaged it as an urgent appointment due to the potential for a retinal break. Before the pandemic we had invested in a Zeiss Cirrus ultra-widefield camera which has been absolutely invaluable in reducing the close contact time at the slit lamp, as well as providing fantastic images for our records and for the referral. We also feel that in this case the eye plan scheme that the patient is a member of was instrumental in encouraging her to seek care.What did you identify during the consultation and what was your reaction?
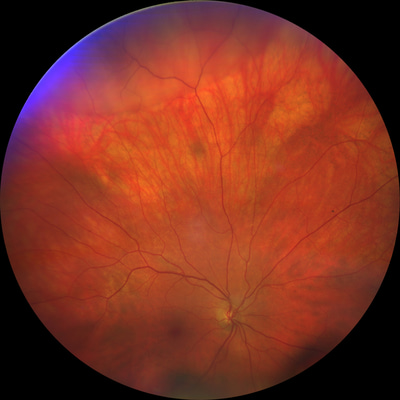
A scan of patient LB’s eye revealing a retinal detachment
How did you approach explaining what you had identified?
MS: It is important not to unduly worry the patient whilst impressing upon them the necessity of immediate treatment. I explained that I had found a small retinal tear and that it would require treatment, but that the detachment had not yet progressed to a point where it was affecting the vision and that with treatment it should be able to be repaired. I showed the patient the images to aid the explanation of what had occurred as patients find it much easier to process in that way. I then explained that it was essential that this was done as soon as possible to prevent the retina detaching further and that I would be referring her immediately to the local eye hospital department for an opinion from a vireo-retinal specialist.What were the next steps that you took, and what was the significance of these steps to this case?
MS: We immediately contacted the ophthalmologist on call to explain our findings and sent the patient for an appointment the same day. It is essential to get cases like this seen as soon as possible as, left untreated, the retina could have detached completely leading to significant and permanent loss of vision.When did you hear about the results of your referral and how have you been involved since?
MS: We called the patient after the weekend as we usually do with any emergency referrals to check how she had got on and to offer any further advice if it was required.What would be your three top tips to other practitioners when making a referral, either generally or during COVID-19?
- Never ignore flashes and floaters, even if the symptoms seem trivial or have resolved. There is often very little correlation between symptoms and the presence of a tear
- Always make clear which is the primary complaint and the urgency of the referral
- Invest in imaging and use it to diagnose problems, support your referral, and justify your decision making.
*The patient’s name has been changed to respect their request for anonymity.
Advertisement


Comments (0)
You must be logged in to join the discussion. Log in