- OT
- Industry
- Equipment and suppliers
- Care with confidence
Advertorial
Care with confidence
Heidelberg Engineering has a passion to help community optometrists deliver confident clinical decision making every time and embrace primary care in partnership with hospitals
Advertorial content is paid for and produced by a sponsor, and is reviewed and edited by the OT team before publication.
29 October 2017
The ageing population, reduced NHS budgets and expanding raft of new treatments available to NHS patients are a few of the unprecedented number of challenges increasing the pressure on Hospital Eye Services (HES) in recent years.
It is predicted that the number of people living with sight loss will increase by a third between 2016 and 2030 to more than 2.7 million1 and recent research suggests an increase in demand over the next 10 years of 25% for cataract services, 30% for medical retina services and 22% for glaucoma services.2
With the population aged 60 or over growing at around twice the rate of the number of ophthalmologists, there is an ever widening gap between supply and demand3 and >90% of HES’s estimate they will require one to five additional consultant ophthalmologists over the next two years.4 The UK already operates with fewer ophthalmologists pro rata than any other nation in the European Union, with around two ophthalmologists per 100,000 population in the UK compared to, for instance, more than 14 ophthalmologists per 100,000 population in Greece.5

Unfortunately, NHS budget cuts and the current government position of freezing the number of training posts for the next 10 years makes balancing the ratio of patients and ophthalmologists an unlikely scenario.
NHS England launched a ‘Call for Action’ in 2014 outlining the desire to develop a long term and sustainable plan for a more preventative approach to eye health, early accurate detection by primary care services and effective management in the community.
- Community optometrists are the obvious choice for collaboration with secondary care because they are:Trained, qualified, regulated and registered eye care providers
- Equipped with modern examination and diagnostic aids
- Easily accessible to patients.
With the right education and technology, optometrists are well positioned to expand the number of services delivered outside of hospital in the near future.
What optometrists could do
Studies have shown community optometrists to be comparable to HES’s in the monitoring of conditions including glaucoma and age-related macular degeneration (AMD).6,7 One study found there were “no marked or statistically significant differences in the outcome” of care between glaucoma patients followed up by the HES and community optometrists.6 Another study concluded that “optometrists were non-inferior to ophthalmologists with respect to the classification of nAMD lesions” and that “shared care with optometrists monitoring quiescent nAMD lesions has the potential to reduce workload in hospitals.”7
Crucial for the optometrists in this study was the use of optical coherence tomography (OCT).7 OCT assists the optometrist in meeting the NHS demands for early and accurate detection and effective management in the community by introducing a multi-modal imaging approach to diagnosis. OCT devices that provide accurate and repeatable results also aid in the early detection of glaucoma and reduce the number of false positive referrals by building robust evidence of progression over time.
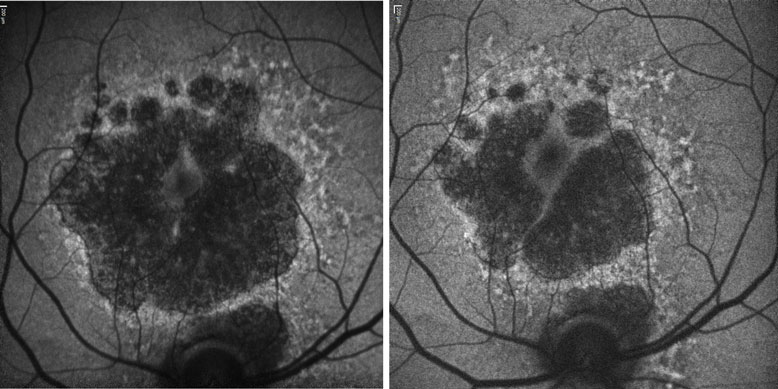
Treatments for dry AMD are on the horizon, with promising phase III trials underway. However, introducing dry AMD treatment would increase the burden on an already strained HES 10-fold. Shared care with optometrists would relieve this burden and be convenient for patients. It is likely that OCT combined with fundus autofluorescence imaging will be essential for the optometrist wishing to take part in dry AMD shared care schemes.
Even as such as obvious choice to deliver shared care, optometrists face significant challenges to integrating new technology into practice, including:
- Return on investment
- Education
- Liability
- WorkflowSpace.
Looking to Heidelberg Engineering for support
Since its inception in 2011, Heidelberg Engineering has focused on educating eye care professionals to facilitate the integration of multi-modal imaging in optometric practice. Whether via clinical peer discussions, workshops, online certification, or onsite team training, Heidelberg Engineering works to build the confidence of everyone in the practice. It is this approach that embeds the technology and yields a return on investment, with every team member embracing the technology and understanding the benefits to the patient.
With HEYEX2 software, integration of a wide range of ophthalmic instruments into a single database is possible, with full connectivity to the electronic medical record and cloud sharing and storage solutions.
Every SPECTRALIS is instantly recognisable because Heidelberg Engineering never sacrifices the core DNA needed for confident clinical decision making. Whether you choose the SPECTRALIS SPIRIT with its 3-click semi-automated workflow, automated report generation and smart iPad review, or the SPECTRALIS SPECIALIST with its scanning flexibility, dynamic visualisation and detailed analysis, TruTrack active eye tracking and retinal recognition allow you to identify the smallest change to as little as one micron of accuracy. And as for space, the SPECTRALIS is surprisingly small and flexible. You can configure your ideal setup with a host of compact table and computer options designed with the smallest of practices in mind.
Heidelberg Engineering is dedicated to providing solutions that equip optometrists to approach primary care opportunities with confidence.
Email [email protected] to find out more.
References
- The State of the Nation Eye Health. Royal National Institute of Blind People. 2016
- The Way Forward Executive Summary. The Royal College of Ophthalmologists. 2017
- Resnikoff, S., Felch, W., Gauthier, T. and Spivey, B. (2012). The number of ophthalmologists in practice and training worldwide: a growing gap despite more than 200,000 practitioners. British Journal of Ophthalmology, 96(6), pp.783-787.
- Workforce Census. The Royal College of Ophthalmologists. 2016
- European Union of Medical Specialists (UEMS)
- Gray, S. (2000). The Bristol shared care glaucoma study: outcome at follow up at 2 years. British Journal of Ophthalmology, 84(5), pp.456-463.
- Reeves, B., Scott, L., Taylor, J., Harding, S., Peto, T., Muldrew, A., Hogg, R., Wordsworth, S., Mills, N., O'Reilly, D., Rogers, C. and Chakravarthy, U. (2016). Effectiveness of Community versus Hospital Eye Service follow-up for patients with neovascular age-related macular degeneration with quiescent disease (ECHoES): a virtual non-inferiority trial. BMJ Open, 6(7), p.e010685.


