- OT
- CPD and education
- Troubleshooting varifocals
Troubleshooting varifocals
Presenting common scenarios outlining how to tackle varifocal non-tolerance cases

Mark Hickton
01 September 2019
In over 20 years of ophthalmic practice, I have seen significant developments in the field of varifocal lenses. With the gradual onset of grey hair and the need for a reading add drawing ever closer, I am beginning to relate more to the visual challenges faced by these patients. As a result of more sophisticated lens designs, adapting to varifocals – or progressive addition lenses (PALs) to use the more technical term – has become a smoother experience for the patient. However, these advances in lens technology also require greater care and attention when taking measurements and fitting. The following cases highlight common areas, which, if handled incorrectly, can lead to patient concerns and possible remakes for the practice.
Case 1
A 51-year-old radiographer who has only had single vision distance spectacles previously: R -1.25 / -0.50 × 5 Add: +1.50 L -1.50 / -0.25 × 180 Add: +1.50
The patient comes in to collect their first-time PALs. The spectacles are adjusted, ensuring that the fitting cross is in the correct position. The temporary markings are removed, and the patient is asked to check their vision. A few seconds later the patient removes the spectacles and utters the dreaded phrase: ‘I’m not sure if I will be able to get on with these.’ After checking the prescription and fitting, the patient is asked to give them another go. However, after trying them on for a further five seconds the patient asks for the spectacles to be changed back to single vision lenses.
In this case we will assume that the prescription and the fitting are correct. So, what has gone wrong? A significant factor in successful PAL dispensing is the management of the patient’s expectations from the outset. First-time wearers must be advised on the limitations and use of PALs to allow them to make an informed decision, taking care to avoid complex jargon. In this particular case, limitations with PALs may be more of an issue for the patient’s close work as it can be observed that the add almost cancels out the distance prescription. In other words, the reading portion of the PAL is very close to plano and it is likely that the patient has previously been used to removing their single vision distance spectacles to read.
Adaption periods of around two to four weeks should be emphasised to first-time wearers
Without their spectacles on, they will have been used to a generous field of view for close work whereas the PAL reading area will be relatively narrow; this should be made clear to the patient during the dispense to manage their expectations in advance of collection.
Adaption periods of around two to four weeks should be emphasised to first-time wearers. Although this approach presents a risk of discouraging some patients from trying PALs, it is important to identify those who are unwilling to compromise to avoid tears and tantrums further down the line. That said, with modern lens designs and good communication during the dispense, patients often find that the lens performance exceeds their expectations on collection and adaption can be much quicker.
Case 2: the tilt effect
A patient comes in with their new PALs, which they have been wearing for three weeks. They report that the distance vision is reasonable, but the near vision zone seems narrow and ‘slightly blurry.’ The patient watches as the dispensing optician takes their spectacles to a mysterious corner of the practice and, on the return of their spectacles, they are asked to check their vision. To their surprise, both distance and reading vision seems to have improved significantly, almost to the point where ‘they seem to be a different pair of glasses.’
This case highlights the importance of the fitting for PALs. An important factor when dispensing PALs is pantoscopic tilt. When designing PALs, manufacturers typically assume a pantoscopic angle of around 8–10° with conventional lenses. Bespoke PALs allow you to order the lenses with very specific fitting measurements including the pantoscopic angle. It is important to note that the pantoscopic tilt is measured with the patient wearing the spectacles and looking straight ahead (see Figure 1) and must not be confused with the angle of side.
Figure 1
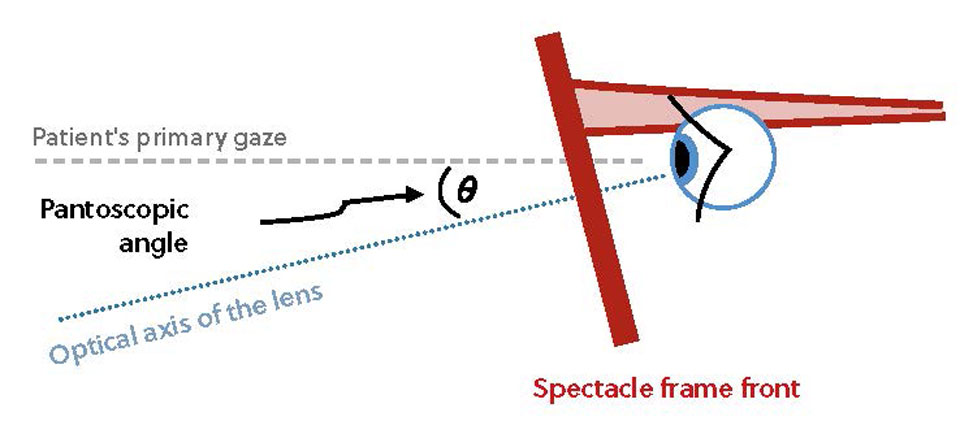
Optimising the pantoscopic tilt helps PAL wearers in a number of ways. The intermediate and reading area of a conventional PAL is significantly narrower compared to the distance portion of the lens. Increasing the pantoscopic tilt brings the near zone closer to the eye, which in turn helps widen the patient’s near field of view due to the ‘keyhole effect.’ Bringing the near zone of the lens closer to the eye also results in the patient looking more perpendicularly through the near portion of the lens which can improve visual performance.
Case 3: the patient with height issues
A patient has come in to your practice with a pair of PALs they collected two weeks ago. The patient can read well, but they feel that their distance vision is not as sharp as their old glasses. The only way the patient gets any noticeable improvement in the distance is by lowering their head.
One of the most common reasons relating to PAL remakes is the measurement of vertical heights. In this case, the fact that ‘the distance vision is better when I drop my head’ should instantly start you thinking about the vertical height position when troubleshooting. Errors can creep into this measurement at the start of the dispense. It is important that the dispenser takes the vertical height measurement when they are at eye level with the patient. The patient’s natural posture may also influence this measurement so the patient must be sat naturally and not slouched back in the chair. If there is any doubt in the height measurements, ask the patient to stand up and view an eye-level target; this precautionary step also helps identify patients who have a naturally elevated head posture. These considerations should also be adopted when using electronic dispensing devices, such as hand-held tablets, to ensure that the camera lens is level with the patient when taking measurements.
To resolve such cases, the PALs should be marked up by identifying the manufacturer’s engravings (see Figure 2) and by using the corresponding PAL template in order to check the fitting cross position on the patient. The dispenser should refer to the manufacturers’ guidelines as to the optimum fitting position. However, it is also worth reviewing the patient’s previous fitting position where applicable, prior to dispensing their new pair.
Figure 2

In this particular case, the solution could be to alter the frame fit to lower the heights, although this can be difficult with plastic frames without adjustable nose pads, and it is important not to compromise the comfort of the frame to achieve this. If the lenses are remade with lower heights, it is important to consider the corridor length of the PAL and the impact this will have on the reading area.
Step-by-step troubleshooting
- Use the engravings to mark-up the PAL, but also to check the lens design/add information
- Always check the lens powers against the prescription, or for modern freeform lenses, the verification powers
- Confirm that the frame is suitable for the dispensed PAL and that the distance and near zones are not compromised
- Look at the patient’s history – check for significant changes in prescription or lens design/fitting
- Use a trial frame with single vision trial lenses to help identify if the problem is with the prescription or the PAL. If the patient still reports visual problems with the trial lenses then a recheck on the prescription should be undertaken
- Has the appropriate PAL been dispensed? Occupational lenses can be better for patients whose near vision is a priority.
Image credit: Shutterstock
Advertisement

Comments (0)
You must be logged in to join the discussion. Log in