- OT
- Professional support
- Clinical and regulatory
- The long view
The long view
How should the education and training of optometrists evolve to future-proof the profession? OT asked optometrists from different modes of practice to share their thoughts

27 October 2020
What will a classroom of optometry students look like in 10 years’ time?
This is particularly pertinent at a time of global upheaval, when practice owners face concerns about keeping their businesses afloat, while many pre-registration and newly qualified optometrists have been left in limbo with the pandemic limiting opportunities for less experienced optical staff.
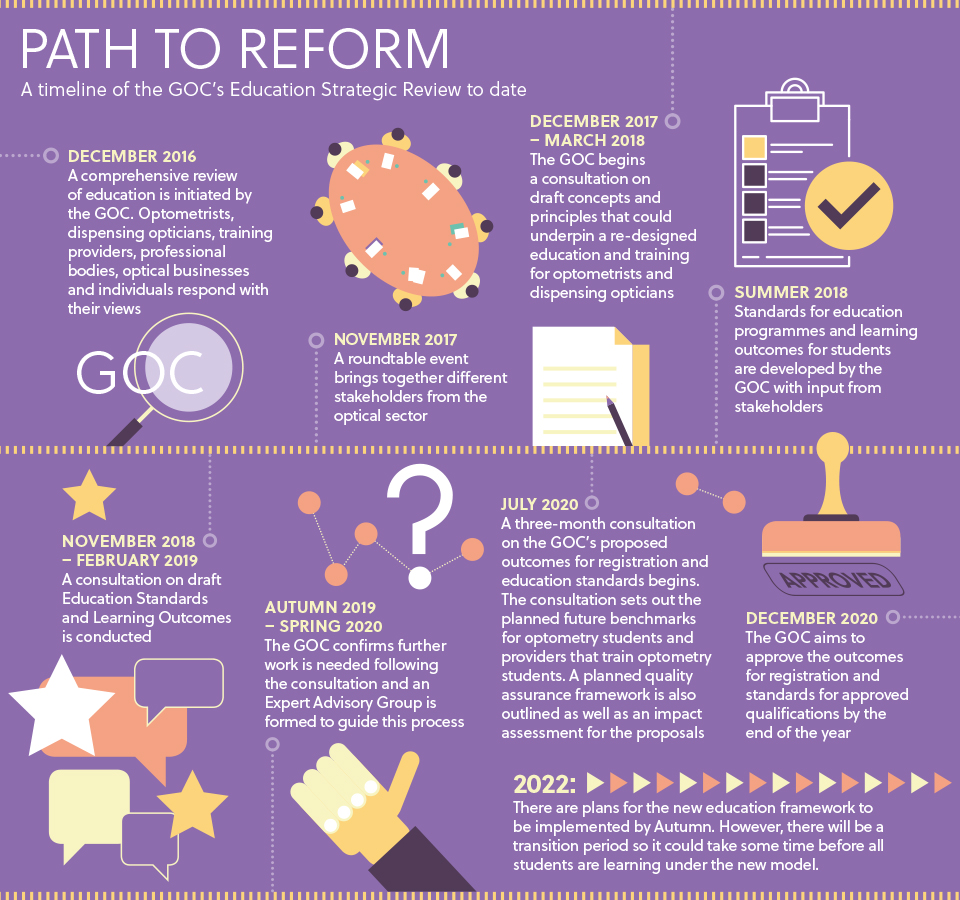
The General Optical Council’s Education Strategic Review aims to re-design the education of optometrists and dispensing opticians to ensure that the optical education system remains fit for purpose as technology and healthcare systems change.
Key planned changes include moving from what, for most students, is a two-stage degree with a pre-registration year to a single-stage approach where one provider is responsible for each student’s education, from the day they start their degree to registration as an optometrist.
The optical regulator plans to move away from a granular, prescriptive approach to one that allows flexibility in how set outcomes are met over the course of a student’s education.
However, concerns have been expressed about how consistency will be maintained across different education providers.
Professional bodies, including the AOP, have also highlighted risks that could result if the new model cannot be adequately funded.
Why change?
Research undertaken by the optical regulator has investigated perceptions of how optical professions will change moving forward and the implications that this has for education.
A 2016 GOC survey of 4139 optometrists, dispensing opticians and optical students found that 87% of respondents thought their role would change significantly within the next five years. Factors that were predicted to influence this shift included technological changes (with 69% of respondents flagging this consideration), an ageing population (55%) and changes in consumer behaviour (54%).
Of the optometrists surveyed, close to half (47%) were involved in the delivery of extended eye care services.
Unless optometrists are eager to upskill and share some of the burden with secondary care under an appropriate funding model, a lot of people could lose vision
The proportion of practitioners offering advanced clinical care varied depending on which country respondents were based in, with 75% of Welsh practitioners involved in offering extended eye care services.
The research also revealed that six in 10 (64%) optometrists had considered gaining additional qualifications to prescribe medicines or assist in the management of patients' eye conditions.
In addition to this research, the optical regulator has explored the views of newly-qualified practitioners on the current optical education system.
A GOC survey in 2018 of more than 700 optometrists who had qualified in the past five years found that 60% of newly qualified optometrists felt there was not enough clinical experience within their academic study.
How should education change?
Technological change, an ageing population and a shift to provide more healthcare services in the community are changing the roles that optometrists and dispensing opticians perform.
But while the impetus for education to adapt to an evolving world is common to all optical professionals, the skills that practitioners value in future optical graduates may vary depending on their perspective and mode of practice.
OT asked optometrists from a range of professional backgrounds for their views on the skills that are necessary to future-proof the profession.
Hospital
Sharing the views of the Hospital Optometrist Committee (HOC), Sheffield Teaching Hospitals optometrist Holly Higgins emphasised that the education of optometrists needs to meet the new demands placed on the profession. This includes being better trained to deal with eye casualties, incorporating independent prescribing into the course and a focus on time management, as well as dealing with stress in the clinical environment.
The HOC suggests that smaller course sizes may help to ensure that students arrive in the workplace with improved practical skills.
“Lastly, communication skills and learning the best and most empathetic way to talk to patients is a key way that training needs to evolve,” Ms Higgins said
Turning to the attributes that are particularly useful in a hospital setting, the HOC emphasise the importance of optical coherence tomography interpretation, although this can be built up over time in-house.

In the experience of HOC members, many students enter pre-reg with limited confidence in the “crucial” skill of assessing the retina using a bio-headset and indirect ophthalmoscopy.
Experience with refraction and retinoscopy for high prescriptions and understanding how this differs to a normal refraction also needs more attention, Ms Higgins highlighted to OT.
A shortage of ophthalmologists has added to the value that hospital optometrists bring to secondary care. Optometrists can become specialised to a very highly skilled level in clinics such as glaucoma, medical retina and corneal clinics.
The HOC notes that some hospital optometrists have branched out into new skillsets, such as carrying out intravitreal injections and performing YAG laser treatment.
The hospital wish list: four key education priorities from the HOC
- Problem-solving. From the start, instead of learning lists of conditions, we should be enabling our students to think through problems, before coming to a diagnosis or decision. Right now, this shift in perspective mainly comes during pre-reg, where a patient will come in with a history, have a clinical examination, and then students learn to piece these bits of information together
- Smaller groups. This could even involve some one-to-one time with students to make sure they learn the clinical skills correctly, so that they leave university confident with things such as Volk. This would set them up much better for pre-registration and their careers
- OCT interpretation. This is a major topic both in hospital and community optometry
- Using hospital experience wisely. Hospital placements offer students the chance to observe how hospital optometry could broaden their knowledge and horizons. Revising topics relevant to a specific clinic makes for a more engaging placement.
Independent prescribing
Birmingham optometrist Don Williams qualified with independent prescribing in April 2019.
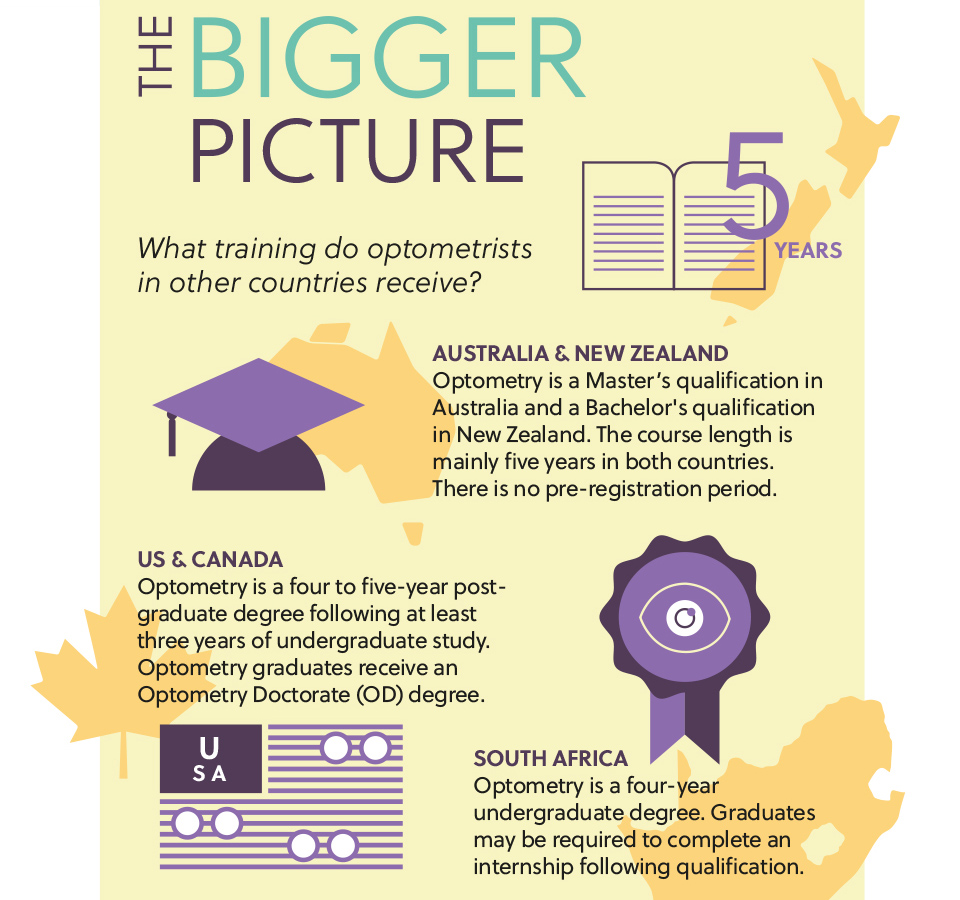
Mr Williams told OT that he believes that students should undertake an additional two years of training to become optometrists – bringing the course closer to the requirements seen in countries such as the US.
He added that in his view the current clinical component of optometry education in the UK
is insufficient. “The programme needs to incorporate more pathology and clinical exposure to these pathologies,” Mr Williams explained to OT.
“A few weeks in a hospital as part of the pre-reg is really not enough,” he added.

Mr Williams would like to see some elements of the current independent prescribing qualification incorporated into the undergraduate education of optometrists in the UK.
To attain the full qualification, optometrists would need to complete a substantial number of clinical hours.
Ultimately, Mr Williams would like to see IP-qualified optometrists work towards a title that has a similar level of respect to that carried by the optometry doctorate (OD) programme in the US and Canada.
“If you have done six or seven years of studying, then that should be reflected in our degree and title,” he concluded.
Domiciliary
Glasgow-based domiciliary optometrist, Stephen Kirley, told OT that the COVID-19 pandemic and new ways of working as a result of the outbreak will have a significant impact on changes to optometric education.
“I think that the lockdown and pandemic have taught us we can do a great deal more of our educational training online,” he said.

In terms of topics that could be covered more thoroughly, Mr Kirley highlighted that a greater awareness of dementia and its effects would be advantageous.
This could be introduced through a dedicated module during the undergraduate education of optometrists.
“We have an ever-advancing life expectancy within our population and dementia is becoming more prevalent as a result,” Mr Kirley told OT.
“Providing as much training in this field as possible would greatly aid practitioner understanding and improve patient management,” he added.
Domiciliary optometrist for the OutsideClinic, Matthew Burford, told OT that the pandemic has “brought into sharp focus the importance of an agile and multi-skilled work force.”

He added that domiciliary optometry is vital, but unfortunately it is often overlooked. The OutsideClinic has worked with universities to raise the profile of the skills required in domiciliary optometry.
“High levels of ‘soft skills’, such as active listening and emotional intelligence, are required as we are often dealing with the most vulnerable members of society,” Mr Burford shared.
“Performers also need to be clinically confident and competent to deal with a range of conditions and investigative techniques within a patient’s home.”
Mr Burford highlighted the need for education and training to be a “career-long journey.”
“Flexibility with ongoing training, such as with a continuing professional development-based system, will allow optometrists and dispensing opticians to focus on their particular areas of skill and interest whilst maintaining core knowledge,” he concluded.
Locum
Optometrist Craig McCoy works as a locum within different Scottish independent practices.
Mr McCoy, who has an independent prescribing qualification, told OT that education and training needs to evolve so optometrists are eye health professionals “first and foremost.”
Practical experience of seeing and treating patients with different eye conditions – including binocular, refractive and pathological conditions – is essential, he emphasised.
“I worked as a resident for four years in a busy multiple before changing and becoming a full-time locum in independent practice,” Mr McCoy said.
“I’m concerned at the trend for optoms to start locum work straight after qualifying,” he added.
Flexibility and a “cool head” are valuable qualities when it comes to working as a locum, Mr McCoy said.
“They only come from experiencing a wide range of patients,” he observed.
Mr McCoy believes that it is important newly qualified optometrists gain experience working in an employed role before exploring working as a locum.
He highlighted that the increased prevalence of eye disease linked to the ageing population and reduced capacity within the hospital eye service following the pandemic has created a “huge backlog” of patients awaiting assessment and treatment.
“Unless optometrists are eager to upskill and share some of the burden with secondary care under an appropriate funding model, a lot of people could lose vision,” he concluded.


Comments (0)
You must be logged in to join the discussion. Log in