- OT
- CPD and education
- Cases from practice
Cases from practice
Experiences of fitting children with contact lenses in High Street independent practice

13 January 2021
Ceri Smith-Jaynes, OT 's clinical editor multimedia editor and an IP optometrist in a High Street independent practice, explains two cases that she's encountered.
Case one
This little girl was nine years old when she first came to my colleague for contact lenses. Despite his deft touch and wealth of experience, they got no further than getting one gas permeable lens on an eye.
Four years on, this self-conscious teenager with a lazy eye wore thick, hyperopic spectacles and walked with her head lowered, hiding behind her fringe:
Refraction
LE +5.75/-1.75 x 170
VA 6/24
VA 6/6
With the passing of time, more soft contact lens options for hyperopes with astigmatism had become available so I fitted her with CooperVision Biofinity torics. She suffered from severe insomnia, so I was particularly keen to use a highly breathable silicone hydrogel material in order to minimise the risk if she accidentally napped in the lenses or wore them late into the night. The lenses sat straight and stable and she managed application and removal herself with a relatively short tutorial.
She continued wear successfully for a couple of years and the effect on her self-esteem was delightful to see. However, in 2019, she said the vision had become variable and her eyes were itching. When asked about her wearing time, she said she wore them daily for about 16 hours. She had purchased some +1.00D reading glasses from a supermarket and was using them at her computer (note: legally, these are not to be sold to under 16s).
The back of her eyelids had become a little lumpy, indicating allergy. It was late Spring, so I decided to treat her for hayfever by prescribing olopatadine eye drops, a combined antihistamine and mast cell stabiliser. These are dosed twice a day, making them advantageous for contact lens wearers compared to over-the-counter alternatives because you can put them in 20 minutes before applying lenses and again after taking them out
I brought her in for a cycloplegic refraction as she hadn’t done this since she was little and she did turn out to be more hyperopic, so I adjusted her contact lens prescription accordingly, allowing her to ditch the ready readers.
The fitting of the lenses still appeared stable and the surfaces clean. The unstable vision could have been a tired child struggling with undercorrected hyperopia or the rough surface on the back of the eyelids moving the lenses about as they dried out at the end of a long day. It’s difficult to know when you change two factors at once. Still, she did report back that she had stopped using the reading glasses and her eyes were feeling somewhat better.
Case two
An eight-year-old boy came with his foster parents for a sight test. He was already moderately myopic, so we had a conversation about the possibilities of myopia control. A year later, his myopia had progressed by a dioptre in each eye.
Refraction
LE -4.00/-0.75 x 10
VA 6/6
VA 6/6
Although we didn’t know his family history, I was concerned about the increasing myopia as his eyeballs grew longer because this can increase the risk of eye disease later in life. He was a good swimmer and attended his local club. Together, with his foster parents, we decided to try EyeDream orthokeratology (ortho-k). This meant he’d be able to wear the rigid lenses overnight, remove them for cleaning and storing in the morning and spend the day free to jump in the pool. The lifestyle advantages were obvious and, without making promises, there was a chance it could slow his myopia progression.
He tolerated the fitting of the lenses remarkably well and managed to apply and remove them himself a few times
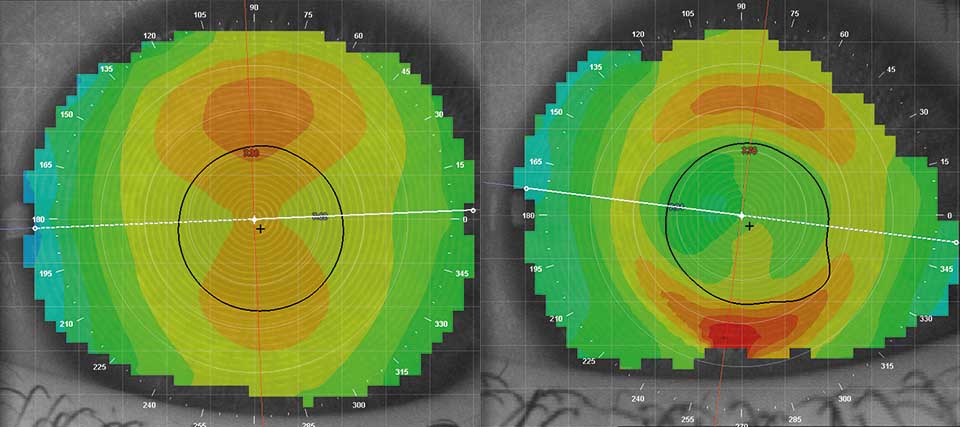
He tolerated the fitting of the lenses remarkably well and managed to apply and remove them himself a few times. I asked him to wear the lenses that night and booked him in first thing in the morning, still wearing them. I checked they weren’t stuck to his cornea and then he removed them in the test room. After just one night his cornea had partially flattened (see Figure 1). I wasn’t expecting his myopia to be fully corrected in one night but, on removing the lenses, he could read some of the letter chart and refraction was less than -2.00D in each eye. After two weeks, we did have to alter the fit of the lenses to help them sit more centrally and to correct his myopia more effectively. The second set of lenses proved effective – he could read the board at school without glasses or contact lenses – and he wore the lenses successfully for the next year.
In that year, his myopia was unchanged in his right eye and had progressed by just half a dioptre in his left eye. His lenses were updated to correct this. This little boy seemed to be flourishing and it was satisfying to be able to help him do well with his competitive swimming.
Ceri’s view…
About the author
Ceri Smith-Jaynes is an IP-qualified optometrist and OT clinical multimedia editor
Advertisement
More Practice team resources: Contact lenses for younger patients
-
Your contact lenses for younger patients resources guide
-
Are contact lenses safe for children?
-
Refraction changes in children
-
On the front line
-
Seeing the benefits
-
Application and removal without the tears and tantrums
-
Introducing contact lenses to kids
-
Contact lenses for younger patients: a guide for every practice


Comments (1)
You must be logged in to join the discussion. Log in
Anonymous31 January 2021
It seems Ortho 'K' is working well in an 8year old; adapting to lenses and handling is remarkable normally would be apprehensive in convincing the parent is always an issue! Anyhow congratulations to achieve success in fitting the myopic child and of course, he will benefit in the control of myopia!
Report Like 296